1679
The value of dynamic contrast-enhanced MRI for discriminating tumor deposition from metastatic lymph nodes adjacent to rectal cancer1The First Affiliated Hospital of Dalian Medical University, Dalian, China
Synopsis
Keywords: Cancer, DSC & DCE Perfusion
Tumor deposits (TD) and N stage are powerful prognostic factors for predicting the overall disease-free survival of rectal cancer patients. However, rectal cancer patients with TD are not the same as those with metastatic lymph node(MLN) in terms of treatment measures and prognosis. TD has similar performance to MLN on conventional CT/MRI images, which makes it difficult to distinguish them. Results of this study indicate DCE-MRI can effectively differentiate TD and MLN adjacent to rectal cancer, and the higher Kep and lower Ve values of rectal cancer with MLN may indicate its’ more aggressive.
Introduction
In recent years, colorectal cancer has become one of the leading causes of cancer-related death, while rectal cancer alone accounts for 30–35% of these cases1. Tumor deposits (TD) are foci of carcinoma separated from the main lesion and identified in pericolonic or perirectal fat or the adjacent mesentery (mesocolonic fat) within the lymphatic drainage area2. Rectal cancer with TD is more aggressive, more prone to metastasis and recurrence, and has a poor prognosis. It is difficult to distinguish TD from metastatic lymph nodes(MLN) on conventional CT/MRI images, TD/MLN are mainly obtained by tumor specimens obtained at the time of surgical intervention. Thus, a method that will enable the pre-operative assessment of cancer with the eventual aim of better assessing prognosis has been long awaited and could be used to tailor individual patient treatment to better combat disease. However, there are few studies on the imaging manifestations of TD. Dynamic contrast-enhanced (DCE) MRI is a functional imaging that can provide valuable information about tumour aggressiveness and the degree of angiogenesis. The purpose of this study is to explore the value of DCE-MRI in differentiating TD and MLN adjacent to rectal cancer.Methods
This study has been approved by the local IRB. 31 patients with pathologically confirmed with rectal cancer were recruited in this study. The patients were divided into two groups: TD group (15 patients) and MLN group (16 patients). They underwent a examination on 3.0T MR (Signa HDxt, GE Medical Systems, USA) with a phased-array body coil. The MR sequences included T2WI, DWI, LAVA, etc. Detailed parameters were listed in Table 1. Ktrans, Kep and Ve maps were calculated from DCE by using GenIQ software at ADW 4.6 workstation. Two radiologists used a double-blind method to place three ROIs on the largest layer of the lesion to measure DCE parameters. The average values were calculated to minimize measurement bias. Mann-Whitney U test or Student’s t test was used to analyze the differences of DCE parameters between the two groups, and the ROC curves were used to evaluate the diagnostic efficacy of these parameters in the differential diagnosis of the two groups.Results
The consistency of the data obtained by the two observers was good (ICC value > 0. 75). The Kep value of TD group (1.50±0.64/min) was significantly lower than that of MLN group (2.16±0.66/min) (P<0.05); the Ve value of TD group [0.43(0.40,0.58)] was significantly higher than that of MLN group [0.32(0.21,0.47)] (P <0.05). The area under the ROC curve (AUC) for the ROC analyses of Kep and Ve for differentiation between TD and MLN groups was 0.773 and 0.739, respectively.Discussion
The significant difference in DCE parameters between the two groups may be due to the greater capillary blood flow and higher cell density in rectal cancer patients with MLN than in those with TD.Conclusion
DCE-MRI may serve as a promising tool for clinical differentiation between TD and MLN, which can help early accurate evaluation and personalized treatment of rectal cancer.Acknowledgements
Not applicable.
References
1. Lee YC, Hsieh CC, Chuang JP. Prognostic significance of partial tumor regression after preoperative chemoradiotherapy for rectal cancer: a meta-analysis. Dis Colon Rectum. 2013;56(9):1093-1101.
2. Lino-Silva LS, Xinaxtle DL, Salcedo-Hernández RA. Tumor deposits in colorectal cancer: the need for a new "pN" category. Ann Transl Med. 2020;8(12):733.
Figures
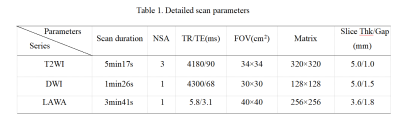
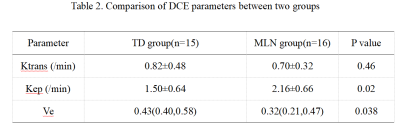
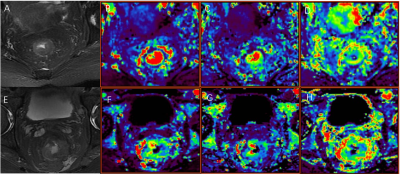
Figure 1. A 80-year-old female, rectal cancer with MLN. The T2WI(A), Ktrans (B), Kep (C), Ve (D) maps were shown, Ktrans, Kep, Ve values are 1.31/min, 1.95/min, 0.40, respectively.
A 69-year-old male, rectal cancer with TD. The T2WI(E), Ktrans (F), Kep(G), Ve(H) maps were shown, Ktrans, Kep, Ve values are 0.57/min, 1.49/min, 0.76, respectively.