1670
Deep Learning Reconstruction: Capability for Image Quality and Staging Accuracy Improvements on Chest MRI in NSCLC Patients1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Fujita Health University Hospital, Toyoake, Japan, 5Fujita Health University School of Medicine, Toyoake, Japan, 6Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan
Synopsis
Keywords: Cancer, Lung, Staging
Deep learning reconstruction (DLR) has been applied in routine clinical practice and started to demonstrate its’ potential in different MR examinations. However, no one have evaluated the utility of DLR for chest MRI, yet. We hypothesize that DLR method is useful for chest MRI and improve image quality and diagnostic performance for T and N factor evaluations in non-small cell lung cancer (NSCLC) patients. The purpose of this study was to determine the influence of DLR method on image quality and diagnostic performance for T and N factor evaluations at chest MRI in NSCLC patients.Introduction
Chest MR imaging (MRI) had been applied at the limited clinical situations since the publication of Radiologic Diagnostic Oncology Group (RDOG) report in 1991. In 2020, Fleischner Society repositions chest MRI as not only academic, but also clinical practices and suggest that one of the best indications is TNM staging for lung cancer (1-3). For chest MRI, conventional parallel imaging (PI) has been widely applied for improving temporal and spatial resolutions in routine clinical practice since 2004. Recently, compressed sensing (CS) has started to be applied for not only brain MRI, but also head and neck or pelvic MRIs (4, 5). In addition, commercially available deep learning reconstruction (DLR) has been applied in routine clinical practice and started to demonstrate its’ potential in different MR examinations (4, 6). However, no one have evaluated the utility of DLR for chest MRI, yet. We hypothesize that DLR method is useful for chest MRI and improve image quality and diagnostic performance for T and N factor evaluations in non-small cell lung cancer (NSCLC) patients. The purpose of this study was to determine the influence of DLR method on image quality and diagnostic performance for T and N factor evaluations at chest MRI in NSCLC patientsMaterials and Methods
Thirty-nine consecutive NSCLC patients (29 male and 10 females; mean age 71 years, age ranged from 56 to 86) underwent chest MRI, surgical resection and pathological examination. All MR examinations were performed at a 3T MR scanner (Vantage Centurian: Canon Medical Systems Corporation, Otawara), and all chest MR data were reconstructed with and without DLR method. In this study, black-blood T2-weighted imaging (T2WI) and short TI inversion recovery (STIR) imaging, pulmonary MRI with ultra-short TE (UTE-MRI), unenhanced and contrast-enhanced 3D T1-weighted (T1W) fast field echo sequence with double fat suppression technique (Quick 3D: Canon Medical Systems) with and without CS were obtained. Then, each data was reconstructed with and without DLR. Black-blood T2WI, STIR and unenhanced and contrast-enhanced Quick 3D without CS were reconstructed as 5mm contiguous section thickness with and without DLR, and UTE-MRI and unenhanced and contrast-enhanced Quick 3D with CS (thin-section Quick 3D) were reconstructed as 1mm contiguous section thickness with and without DLR. Standard reference for TNM stage was determined based on radiological and pathological examination results by tumor board. For quantitative image quality comparison between each sequence with and without DLR, signal-to-noise ratios (SNRs) of tumor and chest wall muscle and contrast-to-noise ratio (CNR) between tumor and muscle were assessed by ROI measurements. For qualitative assessments, overall image quality and T- and N-factor evaluations were performed by chest MRI with and without DLR by two investigators, and final score of each image quality evaluation and T and N factors were determined as consensus of two readers. SNRs of tumor and chest wall muscle and CNR between tumor and muscle were compared by paired t-test. Interobserver agreements for overall image quality as well as T- and N-factor evaluations were assessed as kappa statistics with χ2 test. Then, overall image quality was compared each other by Wilcoxon signed–rank test. In addition, agreements for T and N factor evaluation between each MR protocol and standard reference were determined by κ statistics with χ2 test. Finally diagnostic accuracies for T- and N-factor evaluations on each protocol was compared with standard reference by McNemar’s test.Results
Representative case is shown in Figure 1. Comparisons of SNRs and CNR among all protocols are shown in Figure 2. When applied DLR, SNRs of tumor and chest wall muscle on T2WI, STIR imaging and unenhanced thin-section Quick 3D were significantly higher than those without DLR (p<0.05). Interobserver agreements for overall image quality and compared results of overall image quality between each protocol with and without DLR were shown in Figure 3. Interobserver agreements for overall image quality evaluation on all protocols were significant and substantial or almost perfect (0.75≤κ≤0.86, p<0.0001). Overall image quality of T2WI, STIR imaging and unenhanced and contrast-enhanced thin-section Quick 3D showed significant improvement, when applied DLR (p<0.05). Agreements and diagnostic accuracy for T- and N factor evaluations on chest MRIs with and without DLR are shown in Figure 4. Agreements for T factor evaluation on chest MRI with DLR and that for N factor on chest MRIs with and without DLR were significant and almost perfect (0.82≤κ≤0.85, p<0.0001), although agreement for T factor on chest MRI without DLR was significant and substantial (κ=0.75, p<0.0001). There were no significant differences of T- and N-factor evaluation accuracies between chest RI with and without DLR (p>0.05).Conclusion
DLR is useful for improving image quality on some sequences for chest MRI, although it has a little influence to T- and N-factor evaluations in NSCLC patients.Acknowledgements
This study was financially and technically supported by Canon Medical Systems Corporation.References
- Hatabu H, Ohno Y, Gefter WB, et al; Fleischner Society. Expanding Applications of Pulmonary MRI in the Clinical Evaluation of Lung Disorders: Fleischner Society Position Paper. Radiology. 2020;297(2):286-301.
- Schiebler ML, Parraga G, Gefter WB, et al. Synopsis from Expanding Applications of Pulmonary MRI in the Clinical Evaluation of Lung Disorders: Fleischner Society Position Paper. Chest. 2021;159(2):492-495.
- Tanaka Y, Ohno Y, Hanamatsu S, et al. State-of-the-art MR Imaging for Thoracic Diseases. Magn Reson Med Sci. 2021 Apr 29. doi: 10.2463/mrms.rev.2020-0184. Online ahead of print.
- Ueda T, Ohno Y, Yamamoto K, et al. Compressed sensing and deep learning reconstruction for women's pelvic MRI denoising: Utility for improving image quality and examination time in routine clinical practice. Eur J Radiol. 2021;134:109430.
- Ikeda H, Ohno Y, Murayama K, et al. Compressed sensing and parallel imaging accelerated T2 FSE sequence for head and neck MR imaging: Comparison of its utility in routine clinical practice. Eur J Radiol. 2021;135:109501.
- Kidoh M, Shinoda K, Kitajima M, et al. Deep Learning Based Noise Reduction for Brain MR Imaging: Tests on Phantoms and Healthy Volunteers. Magn Reson Med Sci. 2020; 19(3): 195-206.
Figures

Figure 1. 71-year-old male patient with invasive adenocarcinoma in the left upper lobe and hilar and mediastinal lymph node metastasis.
When applied deep learning reconstruction (DLR), SNRs of STIR image, T2WI and unenhanced thin-section Quick 3D image were significantly improved, although T and N factor evaluations had no difference between MRI with and without DLR. Primary lesion is clearly shown on each imaging, and hilar and mediastinal lymph node metastasis are also clearly shown on STIR and T2-weighted imaging.
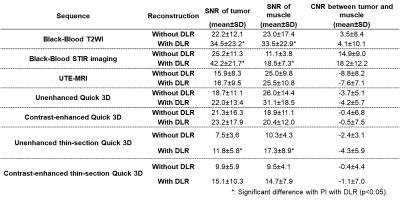
Figure 2. Comparison of results for SNRs and CNR on all sequences.
SNRs of black-blood T2WI, STIR imaging, unenhanced thin-section Quick 3D with DLR were significantly higher than of those without DLR (p<0.05).
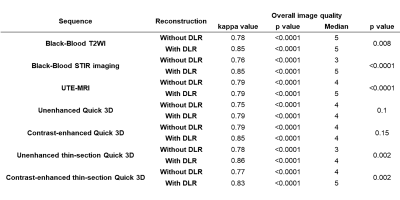
Figure 3. Interobserver agreements for overall image quality and compared results of overall image quality between each protocol with and without DLR.
Interobserver agreements for overall image quality evaluation on all protocols were significant and substantial or almost perfect (0.75≤κ≤0.86, p<0.0001). DLR could significantly improve overall image quality of T2WI, STIR imaging and unenhanced and contrast-enhanced thin-section Quick 3D (p<0.05).
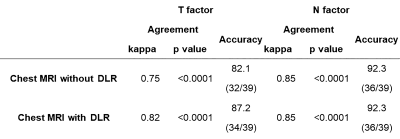
Figure 4. Agreements and diagnostic accuracy for T- and N factor evaluations on chest MRIs with and without DLR.
Agreements for T- and N-factor evaluations on chest MRI with and without DLR were significantly substantial or almost perfect (0.75≤κ≤0.85, p<0.0001). In addition, there were no significant differences of accuracy for T- and N-factor evaluation between chest MRI with and without DLR (p>0.05).