1655
An update of Graded prognostic assessment using molecular markers and Radiomics for estimating survival in NSCLC patients with brain metastases1Department of Radiology, Guangdong Provincial People's Hospital , Guangdong Academy of Medical Sciences, Guangzhou, China, 2Guangdong Provincial Key Laboratory of Artificial Intelligence in Medical Image Analysis and Application, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, China
Synopsis
Keywords: Lung, Radiomics, Prognosis prediction; Non-small cell lung cancer
Rad-molGPA index is prognostic for non-small cell lung cancer patients with brain metastases. The updated Rad-molGPA incorporating radiomics features into the Lung-molGPA is a user-friendly tool to facilitate clinical decision making and appropriate stratification of future clinical trials.Background
Lung cancer is the leading cause of cancer death1, with non-small cell lung cancer (NSCLC) accounting for approximately 85% of lung cancer2. 20% to 30% of patients present with brain metastases at the time of diagnosis. During the disease, approximately 25% to 50% of patients will develop brain metastases3. As systemic therapies for cancer improve, patients with non-small cell lung cancer (NSCLC) live longer and thus are at increased risk for brain metastases4. Thus, understanding how prognosis varies across this heterogeneous patient population is essential to individual care and design future clinical trials5-7. In this study, we aim to develop and validate a scoring system to update the current Graded Prognostic Assessment for Lung Cancer Using Molecular Markers and Radiomics analysis (Rad-molGPA) for estimating survival in patient with NSCLC and brain metastases.Methods
We retrospectively analyzed 775 NSCLC patients who were diagnosed brain metastases between December 2014 and September 2021. By using the methods of radiomics analysis, 591 radiomics features were extracted from brain MRI images, and the radiomics-based score (Rad-score) was constructed. Then, multiple Cox regression was used to select and weight the prognostic factors by their hazard ratios. Significant factors were included in the update Rad-molGPA prognostic index. Log rank tests were used to compare adjacent classes and to compare overall survival for each group.Results
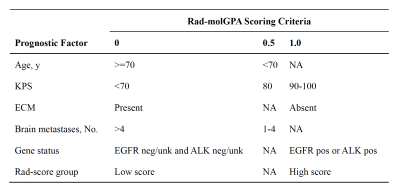
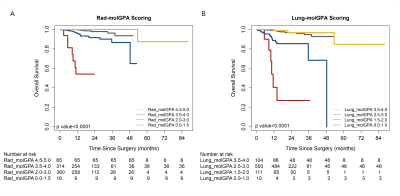
The Rad-score was constructed, which consisted of 7 selected MRI radiomics features. Rad-score successfully classified high-score and low-score patients in discovery dataset (HR: 0.261, 95%CI 0.082-0.835; P=0.001) and validation dataset (HR: 0.198, 95%CI 0.067-0.589; P=0.0004) (Figure 1). The original Lung-molGPA was based on 5 factors: patient age, Karnofsky Performance Status, extracranial metastases, number of brain metastases, and gene mutation status. Significant prognostic factors included the original 5 used in the Lung-molGPA index plus Rad-score in the multiple Cox regression for Rad-molGPA index constructing (Figure 2). Survival rates by the 4 prognostic classes are illustrated in the Figure 3. The median overall survival for the cohort in the present study was 17.07 months, and those with Rad-molGPA scores of 4.5 to 5.0 had a median survival of 22.17 months (Figure 3). The Rad-molGPA index outperformed the Lung-molGPA index for the discrimination of OS prediction (C-index=0.775[95%CI 0.771-0.779] in Rad-molGPA and C-index=0.761, 95%CI 0.755-0.767 in Lung-molGPA; P<0.05).Conclusion
The updated Rad-molGPA incorporating radiomics features into the Lung-molGPA is a user-friendly tool to facilitate clinical decision making and appropriate stratification of future clinical trials.Acknowledgements
The authors have no conflicts of interest to declare.References
1. Sung H, Ferlay J, Siegel RL, et al: Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71:209-249, 2021
2. Chen W, Zheng R, Baade PD, et al: Cancer statistics in China, 2015. CA Cancer J Clin 66:115-32, 2016
3. Thomas NJ, Myall NJ, Sun F, et al: Brain Metastases in EGFR- and ALK-Positive NSCLC: Outcomes of Central Nervous System-Penetrant Tyrosine Kinase Inhibitors Alone Versus in Combination With Radiation. J Thorac Oncol 17:116-129, 2022
4. Eguren-Santamaria I, Sanmamed MF, Goldberg SB, et al: PD-1/PD-L1 Blockers in NSCLC Brain Metastases: Challenging Paradigms and Clinical Practice. Clin Cancer Res 26:4186-4197, 2020
5. Sperduto PW, Yang TJ, Beal K, et al: Estimating Survival in Patients With Lung Cancer and Brain Metastases: An Update of the Graded Prognostic Assessment for Lung Cancer Using Molecular Markers (Lung-molGPA). JAMA Oncol 3:827-831, 2017
6. Sperduto PW, Mesko S, Li J, et al: Survival in Patients With Brain Metastases: Summary Report on the Updated Diagnosis-Specific Graded Prognostic Assessment and Definition of the Eligibility Quotient. J Clin Oncol 38:3773-3784, 2020
7. Sperduto PW, Kased N, Roberge D, et al: Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 30:419-25, 2012
Figures