1576
The feasibility of arterial spin labeling imaging of intracranial tumors at 7T
Xiaoxiao Ma1, Kun Cheng1, Chenyang Zhao2, Jianxun Qu3, Chenxi Li1, Runze Li1, Caohui Duan1, Xiangbing Bian1, Danny JJ Wang2,4, and Xin Lou1
1Department of Radiology, Chinese PLA General Hospital, Beijing, China, 2Mark & Mary Stevens Neuroimaging and Informatics Institute, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States, 3MR Collaboration, Siemens Healthineers Ltd., Beijing, China, 4Department of Neurology, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States
1Department of Radiology, Chinese PLA General Hospital, Beijing, China, 2Mark & Mary Stevens Neuroimaging and Informatics Institute, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States, 3MR Collaboration, Siemens Healthineers Ltd., Beijing, China, 4Department of Neurology, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States
Synopsis
Keywords: Tumors, Perfusion
The goal of this study was to assess the feasibility of pseudo-continuous arterial spin labeling (pCASL) at 7T on patients with intracranial tumors. We found that 7T ASL imaging was feasible and had a higher resolution than 3T ASL imaging and therefore, may enable in vivo assessment of subtle changes and provides a valuable tool for early detection and mechanism investigation of neurovascular function impairments in patients with intracranial tumors.Introduction
Perfusion assessment is crucial in diagnosing, classifying, and grading intracranial tumors [1]. Arterial spin labeling (ASL) can measure perfusion non-invasively, quantitatively, and free from radiation [2] and has been widely used in the study of intracranial tumors [3].7T can benefit the practice of ASL from two aspects, the increased signal-to-noise ratio (SNR) and prolonged T1 relaxation time. With 7T ASL, the perfusion status can potentially be visualized more clearly and measured more accurately. However, the practice of ASL at 7T is problematic due to the deteriorated B1 and B0 field, the limited radio-frequency coverage, and the limitation of specific absorption rate (SAR), especially for the pseudo-continuous (pCASL) labeling approach. Recently, with rapid improvement, the practice of pCASL at 7T became feasible. This study performed 7T pCASL on patients with intracranial tumors and compared the perfusion images with those from 3T.Methods
Ethical approval and informed content were acquired before the study. Four patients were enrolled in this study, one with multinodular vascular neuronal tumor, one with recurrent glioma resection, and two with glioma. The examinations were performed using 3T whole-body scanners (GE Discovery MR 750, GE Healthcare, Milwaukee, WI, or MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany), and a 7T whole-body scanner (MAGNETOM Terra, Siemens Healthcare, Erlangen, Germany). Routine protocols (T2w, T2 dark-fluid, T1w, and T1w+C) and ASL sequences were performed. For 3T, the commercialized 3D ASL was used, with the post-labeling delay (PLD) set to 2.0s. For 7T, all the patients received a prototype 2D pCASL. Additionally, the subject with glioma resection recurrence also received a prototype 3D pCASL at 7T and dynamic susceptibility-weighted perfusion imaging (DSC) at 3T. The 7T 2D pCASL were acquired with gradient echo sequence with the following parameters: 11 slices sequentially played out from inferior to superior, acquisition time per slice 150 ms, slice thickness 5 mm, voxel size 2.2x2.2x5.0 mm3, labeling duration 1.5 s, and PLD 2.0s. For 7T 3D acquisition, 24 slices were acquired, slice thickness 4 mm, voxel size 2.2 x 2.2 x 4.0 mm3, the labeling duration 1.5s, and PLD 2.0s.Results
In all the cases, 7T and 3T ASL imaging showed roughly similar perfusion in the lesion region. ASL at 7T had a higher resolution compared with ASL at 3T. 7T ASL showed better details and a clearer margin of the cortical area and tumor region, while 3T ASL had more blurring (Figure1-3). In the case of glioma resection recurrence, the hyper-perfusion area was not distinct with 3T ASL imaging because of the hemorrhage and postoperative changes. But with 7T ASL imaging, the contrast between the lesion and the normal and hyper-perfusion margin were more apparent (Figure 2). Simultaneously, the surgical resection area was better presented with 7T ASL imaging (red arrow in Figure 2). In the case of glioma, the SNR significantly improved on 3D ASL compared with 2D ASL at 7T (Figure 3). Both 7T and 3T ASL showed hyper-perfusion in the lesion area of the right temporal lobe. However, 3T ASL also showed hyper-perfusion in the left occipital lobe, which was not shown on 7T ASL or 3D DSC imaging (Figure 3). 3T ASL may give a false appearance caused by the volume effect due to insufficient resolution.Discussion and conclusion
7T ASL imaging was feasible and had a higher resolution than 3T ASL imaging, especially for cortex perfusion imaging. High-resolution ASL at 7T may enable in vivo assessment of subtle changes and provides a valuable tool for early detection and mechanism investigation of neurovascular function impairments in patients with intracranial tumors. In the future, more experiments will be performed as this study included only four patients due to its exploratory nature.Acknowledgements
None.References
1. Falk Delgado A, De Luca F, van Westen D, et al. Arterial spin labeling MR imaging for differentiation between high- and low-grade glioma-a meta-analysis. Neuro Oncol. 2018; 20: 1450-1461.
2. Luan J, Wu M, Wang X, et al. The diagnostic value of quantitative analysis of ASL, DSC-MRI and DKI in the grading of cerebral gliomas: a meta-analysis. Radiat Oncol. 2020; 15: 204.
3. Troudi A, Tensaouti F, Baudou E, et al. Arterial spin labeling perfusion in pediatric brain tumors: a review of techniques, quality control, and quantification. Cancers (Basel). 2022; 14: 4734.
Figures
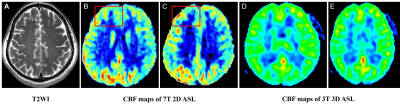
Figure 1. A 55-year-old female patient with
a multinodular vacuolar neuronal tumor in the right frontal lobe on T2WI (A). Cerebral
blood flow (CBF) maps of arterial
spin labeling (ASL) imaging showed hypo-perfusion at both 3T (D and E) and 7T (red
box in B and C). For small lesions, better details of the
cortical region were shown on 7T ASL imaging (red box in B and C) while 3T ASL had
more blurring (D and E).
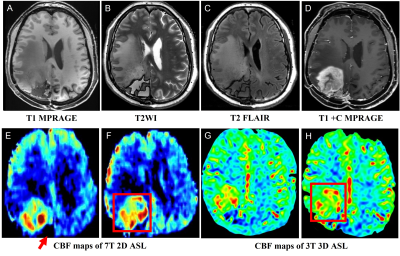
Figure 2. A 63-year-old female patient with recurrent glioma
resection located in the right parietal lobe (A-D). The
hyper-perfusion of the glioma was not distinct on cerebral blood flow (CBF) maps of arterial spin labeling (ASL) imaging
at 3T (red box in H). The contrast between the lesion and the normal brain and the
hyper-perfusion margin were clearer on CBF maps of ASL imaging at 7T (red box
in F). The surgical resection area was better presented at 7T (red arrow in E).
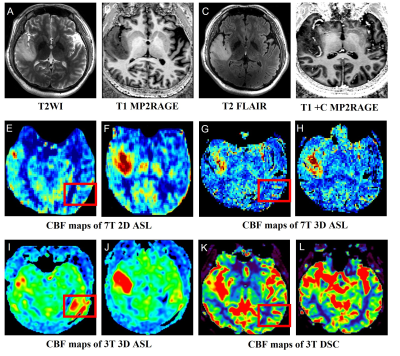
Figure 3. A 46-year-old male patient with glioma in the right
temporal lobe (A-D). Cerebral blood flow (CBF) maps of 7T and 3T arterial spin
labeling (ASL) showed hyper-perfusion perfusion in the lesion area (E-J). However,
CBF maps of 3T ASL also showed hyper-perfusion in the left occipital lobe (red
box in I) which was not shown in CBF maps of 7T ASL and 3T DSC (red box in E, G,
and K).
DOI: https://doi.org/10.58530/2023/1576