1560
Quantitative Analysis of Posterior Decompression in Chiari Malformation by Cine-PC MRI and 3D-T2w Scanning
Xinyu Wang1, Fengtan Li1, Xinli Wang1, Chen Zhang2, and Jianxun Qu3
1Tianjin Medical University General Hospital, Tianjin, China, 2MR Scientific Marketing, Siemens Healthcare, Beijing, China, 3MR Collaboration, Siemens Healthcare, Beijing, China
1Tianjin Medical University General Hospital, Tianjin, China, 2MR Scientific Marketing, Siemens Healthcare, Beijing, China, 3MR Collaboration, Siemens Healthcare, Beijing, China
Synopsis
Keywords: Spinal Cord, Spinal Cord
In this study, the cine-phase contrast (cine-PC) sequence was used to compare the flow rate of cerebrospinal fluid in the midbrain aqueduct of patients with Chiari type I before and after posterior decompression and to analyze the difference in the ratio of cerebellar volume to posterior fossa volume between patients with Chiari type I and normal controls. Cine-PC magnetic resonance imaging and 3D-T2 scanning are shown to be effective for surgically evaluating patients undergoing posterior decompression surgery.Introduction
Chiari type I is a congenital malformation in which cerebellar tonsils descend beyond the defined distance of the foramen magnum, besides other abnormalities related to the anatomical position. Posterior decompression is an effective surgery to treat Chiari malformation.[1] It can enlarge the posterior fossa, reconstruct the cisterna, and allow normal cerebrospinal fluid (CSF) to enter the subarachnoid space. After posterior decompression, the CSF circulation and the pressure gradient at varying levels caused by the CSF flow difference in the spinal canal are improved, thus improving the situation of the cavity in the spinal cord to prevent the expansion of the cavity and shrink the possibility. [2]In this study, we applied cine phase contrast magnetic resonance imaging (cine-PC MRI) and 3-dimensional T2-weighted (3D T2w) imaging for patients with Chiari malformation, aiming to evaluate the CSF flow status and morphological metrics before and after the surgery and establish a quantitative imaging–based approach to assess the surgery outcome.Methods
This study enrolled 20 patients (6 male and 14 female) with Chiari malformation who were admitted to the neurosurgery department between February 2016 and October 2017. Twenty age- and sex-matched participants were also enrolled as controls. The study was performed using a 3T whole-body scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) equipped with a 64-channel head-and-neck phased-array coil. All patients Just in case this makes sense: How do you usually measure the CSF flow? Or do you do it all? And if not: What would be the benefit?underwent routine MRI, 3D T2w-SPACE (imaging-sampling perfection with applied optimized contrasts using varying flip angle evolutions), and cine-PC 1 week before and 6 months after the surgery. The 3D T2w-SPACE sequence was prescribed in sagittal orientation, covering the whole brain, with the following parameters: TR/TE 3200/408 milliseconds, FOV 230 × 230 mm2, resolution 256 × 256, slice thickness 0.9 mm, slices number 172 slices, voxel size 0.9 × 0.9 × 0.9 mm3, and imaging acceleration GRAPPA factor of 2. Two slice positions were prescribed for the cine-PC examination. The first position, transverse, imaged the midbrain aqueducts at the entrances of the fourth ventricle, with the scan lines passing through the hypothalamus and perpendicular to the direction of the CSF flow. The second, sagittal, imaged the median ventricle with a scan line parallel to the interhemispheric fissure. The imaging parameters were FOV = 160 × 160 mm2, phase oversampling = 50%, resolution = 256 × 256, slice thickness = 6 mm, voxel size = 0.6 × 0.6 × 6.0 mm3, acceleration = twofold, and flip angle = 10 degrees. For the transverse position, the velocity encoding (VENC) was 6 cm/s, aligned in the feet-to-head direction, with TR/TE = 24.18/7.71 milliseconds; the acquisition time was 3 minutes 31 seconds. For the sagittal position, the VENC was 20 cm/s, aligned in the foot-to-head direction, with TR/TE = 22.9/7.07 milliseconds; the acquisition time was 3 minutes and 31 seconds. The quantitative analysis index included peak velocity for foot (Vf), for head (Vh), and mean flow (MT) in cine-PC and the cerebellum volume and the posterior fossa volume, and the ratio of the these two volumes in 3D T2w-SPACE. The obtained indexes were statistically analyzed and compared before and after the surgery and compared with those in the control group. A one-way analysis of variance was used to compare the differences. The pairwise t test analysis was performed for pre- and post-surgical data. A p-value less than 0.05 indicated a statistical significance.Results
The PC-magnetic resonance imaging (MRI) sequence indicated that patients with Chiari malformation had reduced CSF flow due to obstruction through the foramen magnum, as indicated by the MT difference between the preoperative group and normal control. After the surgery, the CSF flow was unobstructed, and MT increased whereas Vf and Vh considerably decreased (P < 0.05). No difference was detected between the postoperative and healthy control MT.The 3D T2WI-SPACE sequence revealed no statistically significant difference in cerebellum volume between the preoperative group and normal control (P > 0.05). The differences in the ratio of the cerebellum volume to the posterior fossa volume between the groups were most remarkable (P < 0.01).Conclusions
The MRI cine-PC and 3D T2-SPACE technique can help effectively evaluate the surgical indications of Chiari malformation and the outcome of posterior decompression surgery.[3] At the same time, the decompression of Chiari malformation can increase the flow of CSF in the occipital foramina, slow the CSF flow velocity, and improve the patient's condition.[4]Hence, the decompression of Chiari malformation is a safe and effective surgical method.Acknowledgements
No acknowledgement found.References
[1] Milhorat Thomas H, Misao Nishikawa, Kula Roger W, et al. Mechanisms of cerebellar tonsil herniation in patients with Chiari malformations as guide to clinical management[J]. Acta Neurochirurgica, 2010, 152: 1117-1127.[2] Noudel R, Gomis P, Sotoares G, et al. Posterior fossa volume increase after surgery for Chiari malformation Type I: a quantitative assessment using magnetic resonance imaging and correlations with the treatment response[J]. Journal of Neurosurgery, 2011, 115: 647-658.[3] Aliaga L, Hekman K. E., Yassari R, et al. A novel scoring system for assessing Chiari malformation type I treatment outcomes[J]. Neurosurgery, 2012, 70: 656-664.[4] Yildiz H, Yazici Z, Hakyemez B, et al. Evaluation of CSF flow patterns of posterior fossa cystic malformations using CSF flow MR imaging[J]. Neuroradiology, 2006, 48: 595-605.[5] Bagci A. M., Lee S. H., Nagornaya N, et al. Automated posterior cranial fossa volumetry by MRI: applications to Chiari malformation type I[J]. Ajnr American Journal of Neuroradiology, 2013, 34: 1758.Figures
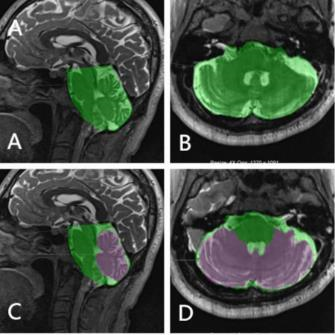
A、B:The volume of posterior fossa was measured in sagittal and axis position .C、D: Cerebellum and posterior fossa volumes were measured in sagittal and axis position position.[5]
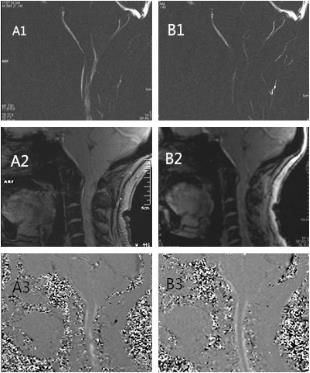
A preoperatively herniated cerebellar tonsil. (A) Preoperative examination images. (B) Postoperative examination images. The foramen magnum was blocked, the spinal cord brainstem was compressed, and obvious syringomyelia was formed. However, the appearance of syringomyelia was no longer seen in the postoperative view, and the spinal cord brainstem pressure was relieved.
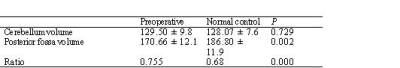
Table 1. Cerebrospinal fluid flow through the foramen magnum, as displayed by the PC MRI sequenceThe flow blocked in 20 patients with Chiari malformation and not smooth after the procedure. The difference was statistically significant (P < 0.05).
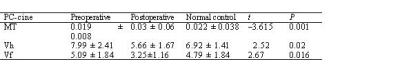
Table 2. 3D T2WI-SPACE sequence resultsNo remarkable difference was observed in cerebellar volume analysis (P > 0.05), but considerable differences were observed in other posterior fossa volumes and the ratio of cerebellar volume to posterior fossa volume (P < 0.05). The ratio of cerebellar volume to posterior fossa volume displayed the most remarkable difference (P < 0.01).
DOI: https://doi.org/10.58530/2023/1560