1554
Nodular change of the cervical nerve root on quantitative double-echo steady-state in cervical spondylosis1Radiology, Chiba University Hospital, Chiba-shi, Japan, 2Diagnostic Radiology and Radiation Oncology, Chiba University Hospital, Chiba-shi, Japan, 3Philips Japan, Tokyo, Japan
Synopsis
Keywords: Spinal Cord, Neuro
Evaluation of intervertebral foramen stenosis is essential in the diagnosis of cervical spondylosis. However, that is not easy because the intervertebral foramen is thin. We focused on the nodular change of the cervical nerve root, which is often visualized in patients with cervical spondylosis. We investigated the relationship between nodular changes and intervertebral foramen stenosis and confirmed the correlation between them. Thus, the identification of the nodular change may be helpful in the diagnosis of cervical spondylosis.Introduction
MRI is used to evaluate nerve root compression and intervertebral foramen stenosis in cervical spondylosis, and it is important to identify the nerve root and compression factors at the responsible level1, 2. In this study, we performed the visual assessment of cervical nerve roots using double-echo steady-state (DESS), which has been reported to be effective in evaluating cervical nerve roots3. Quantitative DESS (qDESS) is a three-dimensional sequence that produces two echoes with different contrast. By adding the two echoes together, a high SNR image with T2 contrast can be obtained4. The two echoes can be separated to obtain quantitative information such as T2 relaxation time. qDESS can delineate the ventral and dorsal roots, but nodular high signal is often visualized in areas where the nerve roots penetrate the dura mater. We hypothesized that the structure reflected nerve root redundancy due to intervertebral foramen stenosis. In this study, we used qDESS to investigate the relationship between the nodular high signal of cervical nerve roots and intervertebral foramen stenosis. Moreover, we measured T2 values of nerve roots.Method
MRI examination: Twenty patients (9 female and 11 male; median age, 69 years [range, 30-83 years]) who underwent cervical spine MRI were included. MRI was performed on a 3.0T unit (Ingenia, Philips Healthcare) using a head and neck-phased array coil. In addition to the conventional cervical spine MRI sequence (sagittal T1-weighted [T1WI], sagittal T2-weighted [T2WI], and axial T2WI), quantitative DESS was performed in the coronal section. Scan parameters are summarized in Table.1.Evaluation: The left and right 3rd~8th cervical spinal nerves (total=240) of 20 patients and the intervertebral foramen through which the target nerves pass were evaluated. The qDESS images taken in the coronal section were reconstructed in the axial section for visual evaluation. The nerve root findings were ranked on a 3-point scale: no nodule, small nodule, and apparent nodule (Figure.1). Intervertebral foramen width was measured in the axial section. T2 values were measured for the seven cases in which a clean T2 map could be calculated. A circular region of interest (ROI) of 3 mm2 was set, and the average value was measured. T2 values was measured in the axial section.
Statistical analyses: The Steel-Dwass test was used to compare the intervertebral foramen widths and T2 values for each group. Spearman's rank correlation coefficient was also used to test whether there was a correlation between the rank of findings in visual assessment and intervertebral foramen width. Statistical significance was set at P < 0.05.
Result
Table 2 shows the results of the visual assessment and measurement of intervertebral foramen width. In the visual assessment, 183, 41, and 16 nerve roots were classified into grade 0 (no nodule), 1 (small nodule), and 2 (apparent nodule), respectively. The lower cervical spine nerves had more nodular changes. The mean ± standard deviation of the intervertebral foramen width for grade 0, 1, and 2 was 4.2 ± 1.0 mm, 3.8 ± 1.1 mm, and 3.0 ± 0.8 mm, respectively. The foramen width narrowed as the nodular change became stronger. The intervertebral foramen widths for each group are displayed in a box plot in Figure 2. Each group had statistically significant differences in intervertebral foramen width. Spearman's rank correlation coefficient was -0.293 (P<0.001).T2 values for each group are displayed in a box plot in Figure 3. The mean ± standard deviation of the T2 values for grade 0, 1, and 2 was 56.9 ± 7.7, 61.4 ± 7.3, and 84.3 ± 6.0, respectively. T2 values higher as the nodular change became stronger. T2 values of grade 2 were significantly higher than other grades.
Discussion
The intervertebral foramen was narrower in the group with more evedent cervical nerve root nodularity. Intervertebral foramen width and nerve root nodular change were significantly correlated. In lumbar spinal canal stenosis, the redundant nerve root, in which the cauda equina nerve root elongates, enlarges, and meanders, is a characteristic finding5. We hypothesized that the nodular change may reflect similar nerve redundancy in cervical intervertebral foramen stenosis. However, pathological support has not been obtained, and congestion and dilation of the venous plexus may also be included in the findings.Furthermore, T2 values were higher in the group with more evedent cervical nerve root nodularity, although the number of cases was limited. Eguchi reported prolonged T2 relaxation time of injured nerve roots in patients with cervical spondylosis6. This suggests that the nodular changes are related to cervical spondylosis.
Evaluation of intervertebral foramen stenosis is essential in the diagnosis of cervical spondylosis, but the intervertebral foramen of the cervical spine is thin and runs oblique to the two-dimensional sagittal and coronal sections that are usually imaged on MRI. Thus, it is sometimes difficult to determine whether it is a true stenosis or a partial volume effect. The results of this study may improve the simplicity and accuracy of identifying intervertebral foramen stenosis by identifying nodular findings, since nodular findings are seen in areas with strong intervertebral foramen stenosis.
Conclusion
There was an association between the nodular change of the cervical nerve roots and intervertebral foramen stenosis. This finding may indicate nerve root redundancy.Acknowledgements
No acknowledgement found.References
- Shedid D, Benzel EC. Cervical spondylosis anatomy: pathophysiology and biomechanics. Neurosurgery 2007; 60(1): S7-13.
- Koga H et al. 3.0 T MR imaging of cervical nerve root in the intervertebral foramen. Spinal Surgery 2008; 22(2): 80-85
- Wang et al. Diagnostic agreement between 3.0-T MRI sequences of nerve root and surgery in patients with cervical radiculopathy. Medicine.2021.100:4
- Jacob et al. Non-contrast MRI of synovitis in the knee using quantitative DESS. European Radiology. (2021) 31:9369–9379
- Jeong et al. Effectiveness of percutaneous lumbar foraminoplasty in patients with lumbar foraminal spinal stenosis accompanying redundant nerve root syndrome. Medicine (2020) 99:33.
- Eguchi et al. Simultaneous MR neurography and apparent T2 mapping of cervical nerve roots before microendoscopic surgery to treat patient with radiculopathy due to cervical disc herniation: Preliminary result. Journal of Clinical Neuroscience. (2020) 74:213-219.
Figures
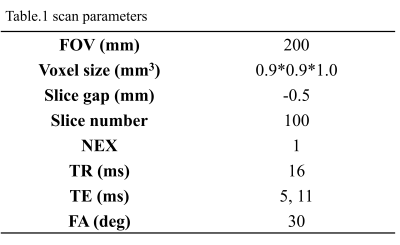
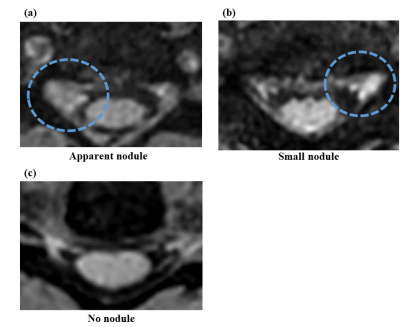
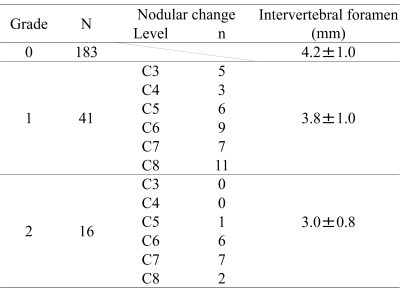
Table.2 Result of visual assessment and intervertebral foramen width. Grade 0=no nodule, grade 1=small nodules, grade 2=apparent nodule. N: Total number of nerve roots. Level, n: The level and number of nerves with nodal changes were shown. Intervertebral foramen widths are presented as mean ± standard deviation.
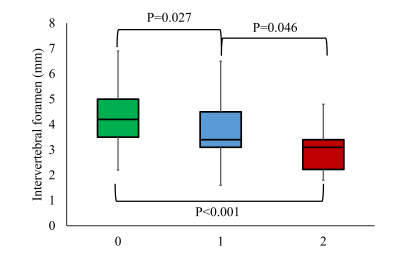
Figure.2 Visual assessment and intervertebral foramen width results were displayed in box-and-whisker plots. The Steel-Dwass test was used to compare intervertebral foramen widths in each group.
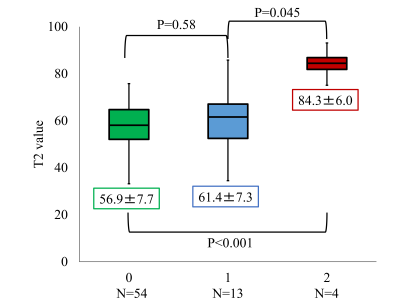
Figure.3 Visual assessment and T2 values results were displayed in box-and-whisker plots. N: The number of nerve roots for which T2 values could be measured. T2 values are presented as mean ± standard deviation. The Steel-Dwass test was used to compare T2 values in each group.