1517
Longitudinal study investigation of CMR measures and cardiac allograft vasculopathy over time
Sandra Quinn1, Chantelle Sanchez1, Ozden Kilinc1, Kai Lin1, Kambiz Ghafourian2, Daniel C Lee2, Esther E Vorovich2, Clyde W Yancy2, Vera H Rigolin2, Jon W Lomasney3, Bradley D Allen1, James C Carr1, and Michael Markl1
1Department of Radiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 2Department of Medicine, Division of Cardiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 3Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States
1Department of Radiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 2Department of Medicine, Division of Cardiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 3Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States
Synopsis
Keywords: Myocardium, Transplantation, cardiac allograft vasculopathy
CAV is a leading cause of mortality in HTx patients. Diagnosis and grading of CAV is dependent on repeated ICA which carries risk of major complications. CMR has the potential to be useful in CAV surveillance without the risk of ICA. This study has demonstrated that in a group of long-term heart transplant patients with evidence of CAV progression who undergo serial CMR and ICA within a close timeframe, 2D global peak strain parameters and 2D systolic strain rate correlates with CAV severity grade. FTS may therefore prove useful for surveillance of patients for CAV.Introduction
Cardiac Allograft Vasculopathy (CAV) is a leading cause of mortality in long-term follow-up of heart transplant (HTx) recipients1. Invasive coronary angiography (ICA), combined with right heart catheterization and echocardiographic parameters, are used as the ‘gold standard’ for surveillance and grading of CAV2. ICA is however associated with risk of major complications and cumulative radiation exposure from repeat procedures3. Cardiac MRI (CMR) has potential for non-invasive surveillance of CAV without the risks associated with ICA. This study used comprehensive cardiac structure-function CMR to evaluate diagnostic value of several CMR measures for non-invasive assessment of CAV severity, including global cardiac left ventricular (LV) and right ventricular (RV) function, T2, T2, ECV and two-dimensional (2D) feature tracking strain (FTS).Methods
This study was approved by the institutional review board and written informed consent was obtained from all patients. 128 adult patients who received orthoptic HTx >1 year prior to enrolment were prospectively recruited from August 2014 to March 2019. Patients with history of humoral rejection or cellular rejection grade ≥2R (n=23), <2 CMR performed (n=23), or CMR without an ICA performed within 9 months of the CMR (n=66) were excluded. 16 patients were thus identified as having each undergone 2 CMR since Htx with a corresponding ICA within 9 months.CMR were performed on a 1.5-T MR system (Magnetom Aera or Avanto, Siemens, Erlangen, Germany). Quantification of global cardiac function parameters was assessed in 32 CMRs using 2D cine-balanced steady-state free precession images. Contouring of LV/RV endocardium/epicardium were contoured manually and excluded trabeculae and papillary muscles. Global native T1 and T2 values were calculated based on the average of all segmental values as per 16-segment American Heart Association model. Native and post contrast blood pool were contoured manually. ECV was calculated as: ECV=(Δ[1/T1myocardium]/Δ[1/T1bloodpool]x[1 -haematocrit]). 27 of 32 CMRs were deemed suitable for FTS analysis. 2D global radial, circumferential and longitudinal peak strain (GRS, GCS and GLS, respectively) and systolic and diastolic strain rate, were evaluated with automated FTS post-processing software (CVI42, Circle Cardiovascular Imaging, V5.13). ICA images, right heart catheterization and echocardiographic data were graded from CAV0 (non-significant) to CAV3 (severe) as per ISHLT criteria2. ICA evidence of disease progression was defined as any new luminal irregularity in a major or 1st degree branch coronary vessel, or change in grade of lesion (e.g. mild to moderate).
Descriptive statistics for continuous variables are presented as mean ± SD, and categorical variables as counts with percentage. Repeat measures were compared with paired t-test (parametric) or Wilcoxon Signed Rank Test (non-parametric). Correlation co-efficient analyses were performed with Pearson (parametric) or Spearman (non-parametric) tests (IBM SPSS Statistics V25.0). P<0.05 was considered statistically significant.
Results
CMR1 and CMR2Patients at the time of first CMR (CMR1) had a mean time from Htx of 8.5 ± 5.7 years, and for repeat CMR (CMR2) of 10.3 ± 6.2 years. At CMR2, patients had significantly reduced LV systolic function (51.3 ± 14.0% vs 59.1 ± 9.4%, P<0.005), LV stroke volume (57.7 ± 33.9ml vs 66.2 ± 25.8ml, P<0.05), RV systolic function (39.1 ± 13.3% vs 44.0 ± 12.8%, P<0.05) and RV stroke volume (53.3 ± 27.7ml vs 62.6 ± 28.4ml, P<0.05) when compared with CMR1. LV end-systolic volume was significantly increased in CMR2 vs CMR1 (55.6 ± 20.6ml vs 51.0 ± 29.8ml, P<0.05). Native T1, T2 and ECV were unchanged between CMR 2 and 1 (Table 1). Most patients at CMR1 were CAV grade of 0 (non-significant) or 1 (mild), with ICA evidence of disease progression by CMR2 in 68.7% of patients, and an increase in severity grade by 1 or more in 50% of patients (Table 1).
CMR1 and CMR2 strain
2D-GRS were reduced at CMR2 when compared with CMR1 (20.7 ± 8.6% vs 25.2 ± 8.5% (SAX); 15.3 ± 7.6 ± 17.5 ± 12.1% (LAX), P<0.05). 2D-GCS was reduced at CMR2 vs CMR1 (-13.2 ± 4.5%, -15.8 ± 3.6%, P<0.05). 2D-GLS values were not significantly reduced at CMR1 vs CMR2 (-10.4 ± 9.0%, -10.3 ± 3.9%, P=0.06). 2D global circumferential peak systolic strain rate (-0.8 ± 0.4 vs -1.0 ± 0.2, P<0.05) and 2D global longitudinal peak systolic strain rate (0.4 ± 0.6 vs 0.8 ± 0.2, P<0.01) were significantly reduced at CMR2 vs CMR1 (Table 2).
Correlations
CAV severity at CMR2, and all CMRs combined, correlated with reductions in LV systolic function, LV cardiac output and LV stroke volume (Table 3). 2D global peak strain in all 3 planes at CMR2 and all CMR combined correlated with CAV severity grade: 2D-GRS (r=-0.61, P<0.005(SAX); -0.46, P<0.05(LAX)), 2D-GCS (-0.62, P<0.005), and 2D-GLS (0.45, P<0.05) (Table 4). In addition, 2D systolic strain rate correlated with CAV severity in all planes: 2D global radial peak strain rate (r=-0.52, P<0.01(SAX); -0.55, P<0.01(LAX)), 2D global circumferential peak strain rate (-0.47, P<0.05), and 2D global longitudinal peak strain rate (0.49, P<0.01) (Table 4). Loss of strain (delta values between CMR1 and CMR2 for 2D-GLS) correlated with angiographic evidence of disease progression (r=0.67, P<0.05).
Conclusion
In this study, HTx patients with serial CMR over time demonstrated evidence of attenuated 2D-FTS parameters, which correlated with CAV severity grade at CMR2. 2D-FTS may supplement standard CMR measures for CAV surveillance long-term.Acknowledgements
No acknowledgement found.References
1. Laks JA, Dipchand AI. Cardiac allograft vasculopathy: A review. Pediatr Transplant. 2022;26(3):e14218.
2. Mehra MR, Crespo-Leiro MG, Dipchand A, et al. International Society got Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy-2010. J Heart Lung Transplant. 2010;29(7):717-727.
3. Al-Hijji MA, Lennon RJ, Gulati R, et al. Safety and Risk of Major Complications With Diagnostic Cardiac Catheterization. Circ Cardiovasc Interv. 2019;12(7):e007791.
Figures
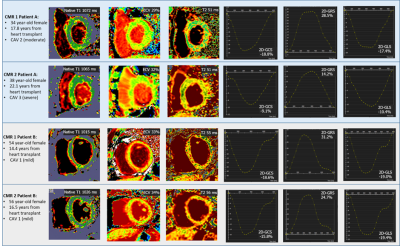
Figure 1: Patient examples of
progressive CAV grade vs stable CAV grade. CMR results are shown of native, T1,
T2, ECV and feature tracking strain parameters of patient A who had progression
of CAV stage over time and B no CAV stage progression over time.
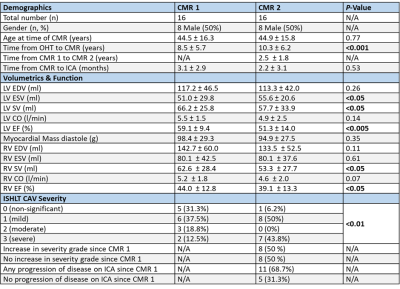
Table 1: Demographics, volumetrics, function,
and CAV severity in heart transplant patients who underwent 2 serial cardiac
MRI with ICA at least 1 year post heart transplant.
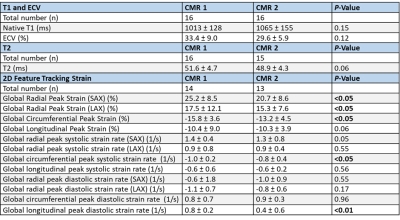
Table 2: Tissue characterization and 2D
feature tracking strain characteristics at CMR 1 and CMR 2.
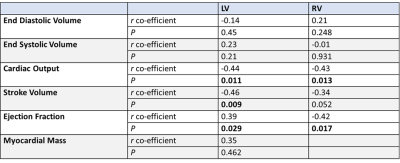
Table 3: Correlation of global structure
and function parameters with CAV severity grade in all CMR studies
performed.
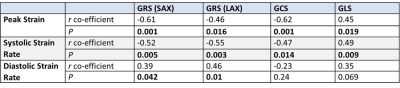
Table 4: Correlation co-efficient analysis for CAV
severity and 2D- feature tracking strain parameters.
DOI: https://doi.org/10.58530/2023/1517