1515
Usefulness of Combined Evaluations of Coronary Calcification and Peripheral Nonenhanced MRA for the Risk Assessment of Future Vascular Events
Seigo Yoshida1, Katsumi Nakamura1, Akiyoshi Yamamoto1, Hidetoshi Akashi2, and Tetsuo Imamura3
1Radiology, Tobata Kyoritsu Hospital, Fukuoka, Japan, 2Vascular Surgery, Tobata Kyoritsu Hospital, Fukuoka, Japan, 3Surgery, Tobata Kyoritsu Hospital, Fukuoka, Japan
1Radiology, Tobata Kyoritsu Hospital, Fukuoka, Japan, 2Vascular Surgery, Tobata Kyoritsu Hospital, Fukuoka, Japan, 3Surgery, Tobata Kyoritsu Hospital, Fukuoka, Japan
Synopsis
Keywords: Atherosclerosis, Cardiovascular
Feasibility of a combined evaluation of coronary artery calcification by plain CT and severity of PAD assessed by nonenhanced MRA was evaluated for predicting the risk of future cerebrovascular and cardiovascular events. The result showed patients who had coronary calcium score of 1000 or higher and more advanced PAD were associated with 67% more subsequent cerebrovascular and cardiovascular events. The possibility of assessing these events in a noninvasive manner has been demonstrated, and early intervention may lead to improved patient outcomes.INTRODUCTION
Coronary artery disease (CAD), cerebrovascular disease (CVD), and peripheral artery disease (PAD) are frequently combined with each other, and there is a disease concept called polyvascular disease1). Polyvascular disease has a high risk of developing cerebral and cardiovascular events, and proactive interventions for CAD and PAD complications have been reported to reduce events within one year.2) Noncontrast-enhanced MR angiogrpahy(NC-MRA)showed excellent diagnostic ability for PAD without radiation exposure and adverse effect of contrast media.3) The purpose of this study was to compare a combined evaluation of coronary artery calcification by plain CT and severity of PAD evaluated by using NC-MRA with subsequent cerebrovascular and cardiovascular diseases, and to investigate the feasibility of predicting the risk of significant arterial events by non-invasive methods.MATERIALS AND METHODS
The study type is a retrospective study with follow-up period of 2007-2022. The subjects were 50 patients (30 males, 20 females, age 50~89;mean age 73.02 years) who underwent both peripheral NC-MRA and chest CT or coronary CT and their subsequent course could be verified in the hospital medical records. Peripheral NC-MRA underwent with use of flow-spoiled FBI (fresh blood imaging) using 1.5T or 3.0T clinical imager. Peripheral arteries were divided into 21 segments (distal aorta, right and left common-, external-, internal- iliac artery, common-, superficial-, deep femoral artery, popliteal artery, anterior-, posterior tibial artery, fibular artery), and the presence of stenosis was evaluated in each segment. Severity of peripheral arterial stenosis of each segment was scored as follows; stenosis more than 50% receiving score 1 and occlusion receiving score 2, then all scores of a patient were summed to obtain peripheral artery disease index (PADI, PAD Index). Coronary calcium score (CCS) was measured with the Agatston method using non-gated chest CT with 1-3 mm slice thickness or gated coronary artery CT with 3 mm thickness. To evaluate correlation between CCS and PADI, the patients were divided into 3 groups according to CCS; group 1 had CCS from 0 to 99, group 2 from 100 to 999, group 3 more than 1000. The patients were also divided into two groups according to PADI; group 1 had PADI less than 5, group 2 had more than 5. Cerebrovascular and cardiovascular events, including stroke, angina, myocardial infarction, and acute heart failure, which occurred after peripheral NC-MRA examination were investigated with electric medical records with follow-up periods from 1 month to 13 years 7 months, 4 years on average. The number of events at PADI from 2 to 4, from 5 to 7, and from 8 to 10 were examined and compared for CCS group 1+2 and CCS group3.RESULTS
The number of patients was 20 in CCS group 1, 14 in group 2, and 16 in group 3. The number of patients was 27 in PADI group 1 and 23 in group 2. There was no significant difference in the PADI between CCS group 1 and group 2 (p=0.93, Fig.1). The PADI in patients of CCS group 3 was significantly higher than that of CCS group 2 (p<0.05, Fig.1). Conversely, CCS in patients with PADI group 2 was significantly higher than that in group 1 (p<0.05, Fig.2). Total of 20 cerebrovascular and cardiovascular events were developed during follow-up periods. In CCS group 1+2, the number of the events were two in PADI from 2 to 4, four in PADI from 5 to 7, and two in from 8 to 10. In CCS group 3, the number of the events were two in PADI from 2 to 4, seven in from 5 to 7, and three in from 8 to 10, (Fig.3). The number of events tends to increase when the PADI is 5 or more, especially the number in CCS group 3 was 67% greater than that in CCS group 1+2.DISCUSSTION
PADI of 5 or more was associated with an increase in the occurrence of subsequent cerebrovascular and cardiovascular events, with the increase being particularly pronounced in cases with CCS of 1000 or higher. Therefore, in cases with severe coronary artery calcification with Agatston score of 1000 or more, the addition of PAD evaluation may help assess the risk of future CVD and CAD events. Contrast-enhanced CTA is currently widely used for the evaluation of PAD, but it is not appropriate for screening due to radiation exposure and adverse effect of contrast media. Although ankle-brachial index (ABI) is highly useful in screening for PAD, hypotension in the affected limb may be mild if the collateral blood vessels are well developed. In this study, PAD was evaluated using FBI, one of the non-contrast MRA techniques. The FBI provides a clear, comprehensive image of the lower extremity without the use of contrast media, making it useful for determining the severity of PAD by indexing the number and degree of stenosis.CONCLUSION
Patients who had coronary calcium score of 1000 or higher and more advanced PAD were associated with 67% more subsequent cerebrovascular and cardiovascular events. The possibility of assessing these events in a noninvasive manner has been demonstrated, and early intervention may lead to improved patient outcomes.Acknowledgements
I would like to thanks Takurou Tahara and Junpei Tanaka.References
1) Bhatt DL, Eagle KA, Ohman EM, et al.;Comparative Determinants of 4-Year Cardiovascular Event Rates in Stable Outpatients at Risk of or With Atherothrombosis. JAMA.2010;304(12:1350-1357)
2) Cacoub PP. Abola MT, Baumgartner I, et al.; Cardiovascular risk factor and outcomes in peripheral artery disease patients in the Reduction of Atherothrombosis for Continued Health(REACH)Registry. Atherosclerosis 2009;204(2:E86-E92)
3) Miyazaki M, Sugiura S, Tateishi F, et al.:Non-contrast-enhanced MR angiography using 3D ECG-synchronizized half-Fourier fast spin echo. J Magn Imaging 2000: 12: 776-783
Figures
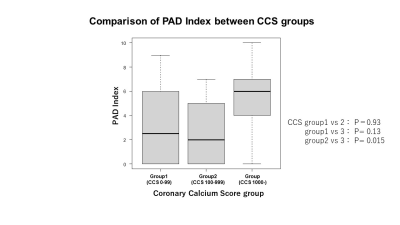
Fig.1 There
was no significant difference in PAD Index between CCS group 1 and group 2 (p=0.93).
PAD Index in CCS group 3 was significantly higher than that of CCS group 2
(p<0.05) .
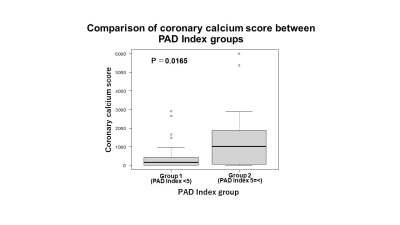
- Fig.2 CCS in patients with PAD Index group 2 was significantly higher than that in group 1 (p<0.05) .
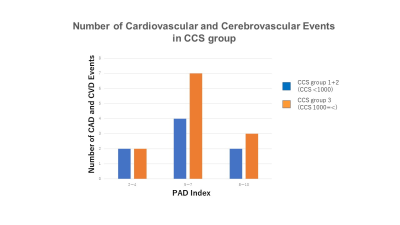
Fig.3 The
number of events tends to increase when PAD Index is 5 or more, especially the
number in CCS group 3 was 67% greater than that in CCS group 1+2.
DOI: https://doi.org/10.58530/2023/1515