1514
High-resolution MR vessel wall imaging combined with Mediterranean diet adherence screener for evaluation of prognosis of ischemic stroke
Xiaochun Wang1 and Wenqiao Zheng1
1First Hospital of Shanxi Medical University, Taiyuan, China
1First Hospital of Shanxi Medical University, Taiyuan, China
Synopsis
Keywords: Atherosclerosis, Stroke
To evaluate the prognosis of ischemic stroke (IS) by plaque characteristics based on high-resolution MR vessel wall imaging combined with Mediterranean diet adherence screener (MEDAS). IS patients were divided into two groups according to their prognosis. Clinical data and plaque characteristics were obtained and compared between groups. The correlation between these characteristics and prognosis was investigated by multivariate analysis. The ROC curves were further performed to determine their predictive performance. NIHSS score, MEDAS score, and plaque enhancement ratio were independent predictors of IS prognosis. Noteworthy, the combined model of three parameters showed significant superiority in the prognosis evaluation of IS.Background
Ischemic stroke (IS) is a common and frequently-occurring disease of the nervous system, which seriously endangers human health and quality of life. Intracranial atherosclerosis and unstable plaques are considered to be the important pathological basis and major causes of IS [1]. Mediterranean Diet (Me-Di), a standard healthy eating pattern, can influence plaque development and progression to further improve the prognosis of IS [2-3]. Thus, plaque characteristics and pre-stroke Me-Di appear to offer additional information for the IS outcome prognostication, but this combined prognostic value has not been evaluated before. Therefore, the purpose of this research was to explore the effects of plaque characteristics by high-resolution MR vessel wall imaging (HRMR-VWI) combined with the Me-Di pre-stroke on the prognosis of IS, and to also determine the valuable predictors related to clinical outcomes.Methods
MCA plaque-induced subacute IS patients with a complete MRI and HRMR-VWI examination were included in the study.Two independent radiologists in cardiovascular radiology and blinded to all clinical information manually contoured the lumen and outer wall boundaries. Then, outer area (OAMLN), lumen area (LAMLN), and wall area (WAMLN) at the site of maximal lumen narrowing (MLN) were automatically obtained. A similar segmentation was drawn in the contralateral normal lumen and the parameters, including OAref, LAref, and WAref at the reference lumen, were also calculated as described above. Finally, the plaque area, degree of stenosis, remodeling index, plaque burden and enhancement ratio were calculated based on the above parameters [4-5].
The adherence to the Me-Di prior to stroke was evaluated with 14-item Mediterranean Diet Adherence Screener (MEDAS). The MEDAS score (range 0 [low adherence] to 14 [high adherence]) was recorded in detail through a complete interview between neurologists and patients or their direct relatives [6]. The National Institute of Health Stroke Scale (NIHSS) score (range 0 [no symptom] to 42 [severe neurologic dysfunction]) of stroke patients within 24 hours after admission was recorded by the neurologist [7]. Furthermore, the clinical outcomes of patients at 3-month after discharge were evaluated using the Modified Rankin Scale (mRS; range, 0 [disease-free] to 6 [dead]) [8]. In addition, age, gender, hypertension, and other disease history were obtained by patient interview and medical records.
SPSS software was used for statistical analysis. All parameters were compared between the groups. To determine the factors related to the poor prognosis of stroke, these parameters (P < 0.05 in comparisons between groups) were further conducted the multivariate logistic regression analysis. The receiver operating characteristics (ROC) curves, as well as the area under curves (AUCs) were further plotted and calculated to evaluate the predictive performance for each parameter. P < 0.05 was considered significant.
Results
A total of 49 patients (34 men and 15 women) with subacute IS were collected. According to mRS results, patients were assigned into two groups, including 25 patients with poor prognosis and 24 patients with good prognosis. The patients with poor prognosis were significantly older than those with favorable outcomes (P = 0.029). In poor prognosis group, the NIHSS score after admission was higher than good prognosis group (P < 0.001). Additionally, other general information did not differ significantly (Figures 1).Among the imaging characteristics of MCA plaque based on HRMR-VWI, the degree of stenosis, plaque burden, and plaque enhancement ratio demonstrated a significant increase in poor prognosis group than in good prognosis group (all, P < 0.001). Statistical differences in other plaque indicators such as plaque area were not found (Figures 1-2).
The distribution of MEDAS scores between the two groups was demonstrated specifically in Figure 3. The median of MEDAS score in all patients was 6 (IQR 3). Among the 24 patients with good prognosis, 83.3% of the patients were highly adherent to the Me-Di (defined as MEDAS ≥ 6), whereas the proportion in the poor prognosis group was only 56% (14 / 25). The univariate analysis further demonstrated that the MEDAS score of poor prognosis patients was remarkably lower than good prognosis patients (P < 0.001) (Figures 1).
Multivariate logistic regression analysis demonstrated that admission NIHSS score (OR: 2.383; 95% CI: 1.095-5.186; P = 0.029), plaque enhancement ratio (OR: 1.379; 95% CI : 1.002-1.898; P = 0.048) and MEDAS score (OR: 0.444; 95% CI: 0.201-0.983; P = 0.045) were significant predictors for evaluating the prognosis of IS, whereas age, degree of stenosis, and plaque burden (all, P > 0.05) were not (Figure 4).
The AUCs of NIHSS score after admission, plaque enhancement ratio, and MEDAS score used to assess the prognosis were 0.818, 0.820, and 0.874, respectively. The combination of plaque enhancement ratio and MEDAS score improved it to 0.902, with sensitivity and specificity of 76.00 % and 91.67 %. Furthermore, the combined model of three parameters resulted in the highest AUC of 0.950, the sensitivity 84.00 %, and the specificity 95.83 % (Figure 4).
Conclusions
In conclusion, NIHSS score, MEDAS score, as well as the plaque enhancement ratio were independent predictors of subacute IS prognosis. Noteworthy, the combined model showed significant superiority in the prognosis evaluation of stroke.Acknowledgements
This study has received funding by the National Natural Science Foundation of China (grant number 81971592), and the Beijing Medical Reward Fund (grant number YXJL-2021-0353-0604).References
[1] GBD 2016 Stroke Collaborators (2019) Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(5):459-480[2] Saulle R, Lia L, De Giusti M, La Torre GJLCt (2019) A systematic overview of the scientific literature on the association between Mediterranean Diet and the Stroke prevention. Clin Ter 170(5):e396-e408
[3] Welty FK (2020) Dietary treatment to lower cholesterol and triglyceride and reduce cardiovascular risk. Curr Opin Lipidol 31(4):206-231
[4] Cruz-Flores SJN (2007) Prospective study of symptomatic atherothrombotic intracranial stenoses: the GESICA study. Neurology 68(3):241-242
[5] Lee H, Ryu C, Yun SJFin (2018) Vessel-Wall Magnetic Resonance Imaging of Intracranial Atherosclerotic Plaque and Ischemic Stroke: A Systematic Review and Meta-Analysis. Front Neurol 9:1032
[6] Fung T, Hu F, McCullough M, Newby P, Willett W, Holmes MJTJon (2006) Diet quality is associated with the risk of estrogen receptor-negative breast cancer in postmenopausal women. J Nutr 136(2):466-472
[7] Lyden P (2017) Using the National Institutes of Health Stroke Scale: A Cautionary Tale. Stroke 48(2):513-519
[8] Broderick J, Adeoye O, Elm JJS (2017) Evolution of the Modified Rankin Scale and Its Use in Future Stroke Trials. Stroke 48(7):2007-2012
Figures
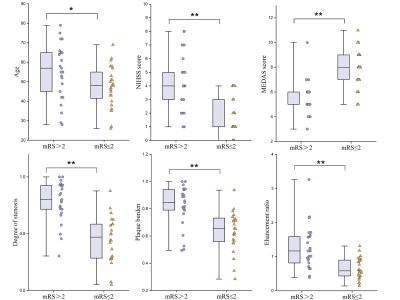
Figure 1. Comparisons of clinical characteristics and MCA plaque characteristics on HRMR-VWI in two groups. *P<0.05, **P<0.01.
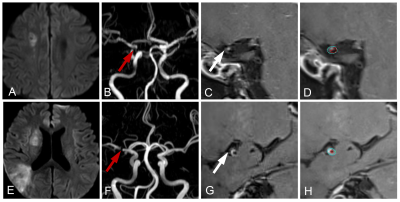
Figure 2. Representative cases. A~D, a 51-year-old man, mRS score 0, MEDAS score 9, NIHSS score 2. DWI showed subacute infarcts (A). MRA showed mild stenosis of the right MCA (B). 3D CE-T1-SPACE showed plaques (C~D). E~H, a 42-year-old man, mRS score 3, MEDAS score 6, and NIHSS score 3. DWI showed subacute infarcts (E). MRA showed severe stenosis (F) in the right MCA, and plaque (G~H) on 3D CE-T1-SPACE.

Figure 3. The distribution of MEDAS
score between the two groups.

Figure 4. Receiver
operating characteristic (ROC) curves of individual factors and combined model,
and odds ratio (OR) and 95% CI based on multivariable logistic regression for
each factor.
DOI: https://doi.org/10.58530/2023/1514