1507
Relationship beween Plaque burden, calcification features and low carotid stent expansion rate by high-resolution MR vessel wall imaging1Radiology, Beijing Anzhen Hospital, BeiJing, China, 2Philips Healthcare, BeiJing, China
Synopsis
Keywords: Vessel Wall, Atherosclerosis
To quantitatively evaluate carotid plaque burden and components and to explore the association between carotid plaque burden and compositions and carotid stent expansion rate (SER) by using carotid high-resolution magnetic resonance vessel wall imaging (HR-VWI). Maximum wall thickness (OR 1.75; 95% CI, 1.02-3.00, P=0.04), maximum single-slice calcification circumference score (OR 2.79, 95% CI 1.06 - 7.37, P=0.03), and maximum area percentage of calcification (OR 1.20, 95% CI 1.04 - 1.39, P=0.01) as predictors of the low SER. Larger culprit plaque, larger calcification area, and greater calcification circumference were independently associated with a low SER after carotid artery stenting.Introduction
Carotid artery stenting (CAS) has emerged as a valid alternative to carotid endarterectomy (CEA) in high-surgical-risk patients. Residual stenosis is an independent risk factor for restenosis, which can affect the long-term outcome after stenting 1,2. A recent study showed that plaque morphology, calcified plaque, and stent type are risk factors for residual stenosis. In addition, a low stent expansion rate was also associated with the development of residual stenosis 2. The stent expansion rate (SER) is defined as the difference between the preoperative stenosis rate of the carotid artery and the residual stenosis rate post-stenting, reflecting the expansion ability of the stent2. High-resolution magnetic resonance vessel wall imaging (HR-VWI) has been widely used to evaluate the carotid plaque burden and component 3,4. It is also an excellent method for assessing calcification with an accuracy of 98% and a specificity of 99% 5. However, the effect of carotid plaque burden and composition on SER remains unknown. Our study aimed to quantitatively evaluate carotid plaque burden and components by carotid HR-VWI and to explore the association between carotid plaque burden and compositions and SER.Methods
A total of 89 patients (mean age, 70±8 years; 69 men) were included in the final analysis. The median SER for 89 patients was 49.2%. Patients were divided into the low stent expansion rate (LSER) (SER≤49.2%) and the high stent expansion rate (HSER) groups (SER>49.2%). All patients underwent preoperative carotid HR-VWI and quantitative plaque burden and composition analysis. MR examinations were performed on a 3.0T MR scanner (Ingenia CX, Philips Healthcare, Best, the Netherlands). Scanning sequences were as follows: T1WI [repetition time (TR)/echo time (TE): 800/10 ms], T2WI (TR/TE: 4,800/50 ms), time of flight (TOF) (TR/TE: 20/4 ms), and simultaneous non-contrast angiography and intraplaque hemorrhage (SNAP) (TR/TE: 12/6.8 ms). Post-processing was analyzed using commercialized software (Vessel Explorer 2, TSimaging Healthcare, Beijing, China) by two experienced reviewers (W.Yu, and YM. S, radiologists with 20 and 3 years of experience, respectively). Lumen boundaries, wall boundaries,and plaque components were manually outlined section by section. SPSS software (25.0) was utilized for evaluating statistical analysis results. The clinical records and HR-VWI imaging features were compared between the two groups by using the independent t test, the wilcoxon rank sum test, and the chi-squared test. Logistic regression analyses were performed to determine the independent factors associated with the LSER. The receiver operating characteristic curves (ROCs) were plotted; the area under the curve (AUC) and cutoff value was calculated for factors with independent significance.Results
Among 89 patients, 46 (51.7%) developed a LSER (Figure1). Baseline and imaging characteristics of the study population are listed in Table 1 and Table 2. The logistic regression analysis detected maximum wall thickness (OR 1.75; 95% CI, 1.02-3.00, P=0.04), maximum single-slice calcification circumference score (OR 2.79, 95% CI 1.06 - 7.37, P=0.03), and maximum area percentage of calcification (OR 1.20, 95% CI 1.04 - 1.39, P=0.01) as predictors of the LSER in Table 3. In addition, the combination of three factors increased the AUC to 0.90 (Figure 2). The cutoff values of maximum wall thickness, maximum single-slice calcification circumference score, and maximum area percentage of calcification were 4.77, 2.5, and 14.53%, respectively.Discussion
Previous studies have shown that the stent expansion is mainly attributable to plaque compression and stretching of the vessel wall 6. Plaque burden and composition can affect stent expansion. The hardness of calcification plaques and larger culprit plaques may resist sufficient plaque compression, which prevents adequate stent expansion 7. Our findings suggest that larger culprit plaques, larger calcification areas, and greater calcification circumferences are associated with LSER. LSER is associated with stent residual stenosis and affects the long-term outcome after stenting. We quantified the carotid plaque features associated with LSER by HR-VWI, which may provide a new consideration for clinicians when performing a surgical strategy.Conclusions
Larger culprit plaque, larger calcification area, and greater calcification circumference were independently associated with a LSER after CAS.Acknowledgements
NoneReferences
1. Daou B, Chalouhi N, Starke RM, et al. Predictors of restenosis after carotid artery stenting in 241 cases. J Neurointerv Surg 2016;8:677-9.
2. Tao Y, Hua Y, Jia L, et al. Risk Factors for Residual Stenosis After Carotid Artery Stenting. Front Neurol 2020;11:606924.
3. Geiger MA, Flumignan RLG, Sobreira ML, et al. Carotid Plaque Composition and the Importance of Non-Invasive in Imaging Stroke Prevention. Front Cardiovasc Med 2022;9:885483.
4. Tapis P, El-Koussy M, Hewer E, et al. Plaque vulnerability in patients with high- and moderate-grade carotid stenosis - comparison of plaque features on MRI with histopathological findings. Swiss Med Wkly 2020;150:w20174.
5. Fabiano S, Mancino S, Stefanini M, et al. High-resolution multicontrast-weighted MR imaging from human carotid endarterectomy specimens to assess carotid plaque components. Eur Radiol 2008;18:2912-21.
6. Elsayed N, Yei KS, Naazie I, et al. The impact of carotid lesion calcification on outcomes of carotid artery stenting. J Vasc Surg 2022;75:921-9.
7. Barrett HE, Cunnane EM, Kavanagh EG, et al. On the effect of calcification volume and configuration on the mechanical behaviour of carotid plaque tissue. J Mech Behav Biomed Mater 2016;56:45-56.
Figures
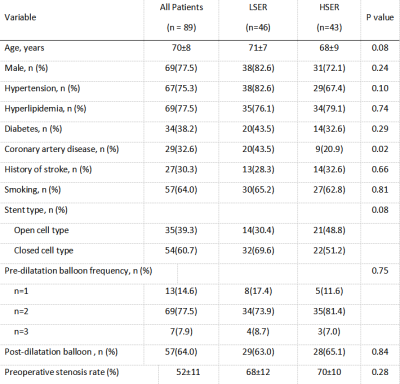
Table 1. Baseline characteristics of the study population
LSER, low stent expansion rate; HSER, high stent expansion rate.
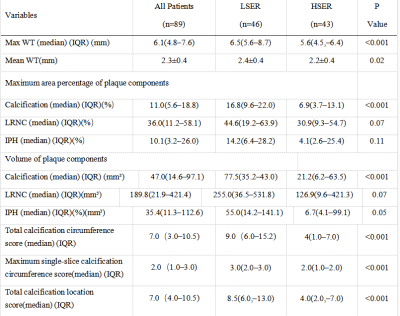
Table 2: Imaging features of the study population
WT, wall thickness; LRNC, lipid-rich necrotic core; IPH, intraplaque hemorrhage; IQR, interquartile range; LSER, low stent expansion rate; HSER, high stent expansion rate.
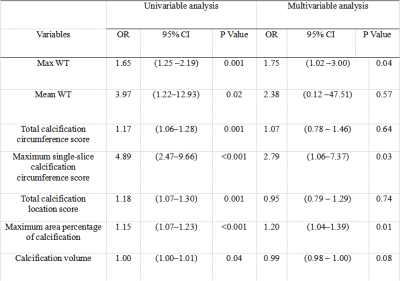
Table 3. Univariable and multivariable analysis to identify imaging features associated with LSER compared with HSER
WT, wall thickness; OR, odds ratio; CI, confidence interval; LSER, low stent expansion rate; HSER, high stent expansion rate.
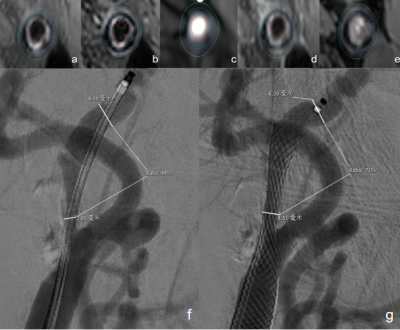
Figure 1. A 79-year-old male patient with a low stent expansion rate.
Images a, b, c, d, and e represent the T1WI, T2WI, TOF, post-contrast T1WI, and SNAP images. Image f shows the preoperative stenosis rate is 56%; image g shows the post-stenting stenosis rate/residual stenosis rate is 29%. The stent expansion rate is 27%. SNAP: simultaneous non-contrast angiography and intraplaque hemorrhage. The green dots and lines indicate vessel walls. The red dots and lines represent vessel lumens. The blue dots and lines indicate the presence of calcification.
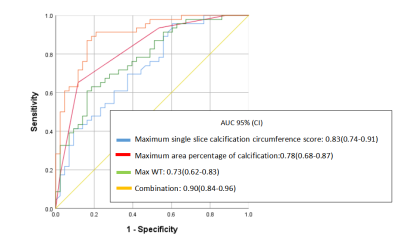
Figure 2. Receiver operator characteristic analysis for imaging features associated with LSER
WT, wall thickness; AUC, area under the curve; CI, confidence interval.