1503
The Added Value of Reduced Field-of-view IRIS-DWI Sequence for T2WI Sequence in T Staging of Rectal Cancer1Xuzhou medical university, Xuzhou,Jiangsu Province, China, 2The affilliated hospital of Xuzhou Medical University, Xuzhou,Jiangsu Province, China, 3Suining Country People's hospital affiliated to Xuzhou Medical University, Xuzhou,Jiangsu Province, China, 4Philips Healthcare, Shanghai Province, China
Synopsis
Keywords: Cancer, Diffusion/other diffusion imaging techniques, diagnosis confidence
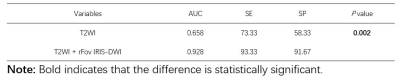
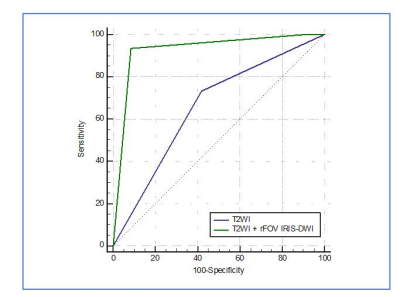
We aimed to evaluate the added value of reduced field-of-view (rFOV) IRIS-DWI sequence for T2WI sequence in evaluating T staging of rectal cancer. ROC analysis showed the diagnosis performance based on T2WI + rFOV IRIS-DWI imaging was superior to single T2WI sequence. The AUC, sensitivity and specificity were 0.928, 93.3%, 91.7% and 0.658, 73.3%, 58.3% for two diagnosis methods respectively. The result showed significant difference between two methods with P = 0.002. rFOV IRIS-DWI combined T2WI imaging could provide higher diagnosis confidence and higher diagnosis accuracy for rectal cancer T staging.Introduction
Oblique axial high-resolution T2WI was the recommended sequence for rectal cancer T staging, according to the guidelines1-3. However, the accuracy of T staging based on conventional T2WI sequence may be influenced by radiologist experience, inflammatory fibrous response, imaging quality, etc4-6. The image reconstruction using image-space sampling function (IRIS) diffusion-weighted imaging (DWI) sequence was a novel technology for high-resolution DWI. Previous study showed that the IRIS-DWI sequence may improve the imaging quality in the female pelvic cavity7. So, we attempted to evaluate the added value of reduced field-of-view (rFOV) IRIS-DWI sequence for T2WI sequence in evaluating T staging of rectal cancer.Methods
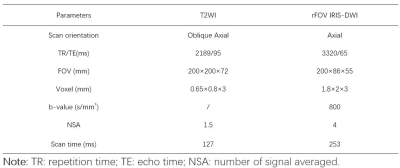
All patients who underwent rectal MRI examinations in our institution between June 2022 and November 2022 were retrospectively enrolled. rFOV IRIS-DWI and oblique axial high-resolution T2WI images were acquired using a 3.0T MR scanner (Ingenia Elition, Philips, Best, the Netherlands) (Table 1). The images were transferred to the Philips IntelliSpace Portal workstation (version V10.1) for evaluation. All patients were evaluated in two rounds by two different methods. First, one senior radiologist (Y.K.M.) with more than 7 years of experience in rectal cancer MRI evaluated the T staging based on oblique axial T2WI high-resolution images and recorded the diagnosis confidence. Second, the same radiologist (Y.K.M.) reevaluated the T staging based on rFOV IRIS-DWI and T2WI high-resolution images after one-week interval. And the diagnosis confidence was also recorded. The radiologist was blind to the detailed pathologic T staging. MedCalc statistical software (version 20.116, MedCalc Software Ltd) was used for data analysis. The accuracy of two diagnosis methods between oblique axial high-resolution T2WI and T2WI + rFov IRIS were compared by paired c-test. Paired sample t-test was used to compare the diagnosis confidence between the two diagnosis methods. ROC curve was used to evaluate the diagnostic performance for pT3 staging. P < 0.05 indicated the difference was statistically significant.Results
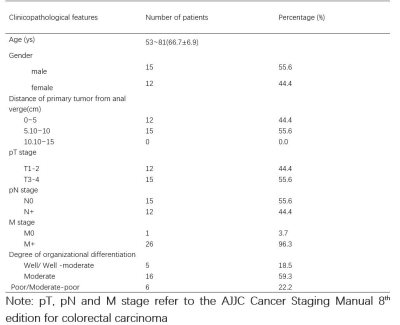
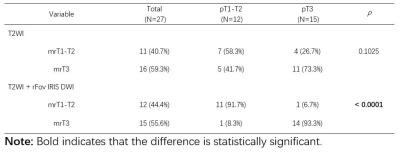
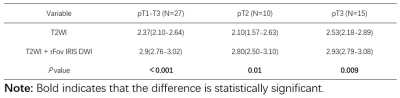
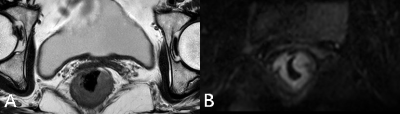
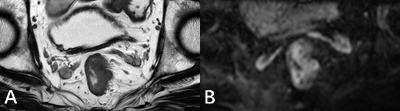
Twenty-seven patients with rectal cancer were enrolled in this retrospective study. The average age of all patients was 66.7±6.9 years, and there were 15 (56%) males and 12 (45%) females (Table 2). The diagnosis accuracy for pT1-pT2 and pT3 was 58.3% and 73.3% according to oblique axial high-resolution T2WI weighted imaging, respectively. Five patients (41.7%) with pT1-pT2 staging were evaluated as mrT3 and four patients (26.7%) with pT3 staging were evaluated as mrT1-T2 (Table 3). According to the oblique axial high-resolution T2WI weighted and rFOV IRIS-DWI imaging, 11 patients (91.7%) were accurately diagnosed in all 12 pT1-T2 staging patients, and 14 patients (93.3%) were accurately diagnosed in all 15 pT3 staging patients. The difference was statistically significant with P value less than 0.0001 (Table 3). Based on T2WI + rFOV IRIS-DWI imaging showed higher diagnosis confidence, and the diagnosis confidence between two diagnosis methods were 2.37 and 2.9 in all patients respectively (P<0.001) (Table 4). For pT2 staging subgroup patients, the diagnosis confidence based on T2WI + rFOV IRIS-DWI imaging also showed higher confidence than single T2WI imaging (2.8 vs. 2.1, P = 0.01). And, for pT3 staging subgroup patients, the P value was 0.009 for two diagnosis methods (2.93 vs. 2.53, respectively) (Table 4). ROC analysis showed the diagnosis performance based on T2WI + rFOV IRIS-DWI imaging was superior to single T2WI sequence. The AUC, sensitivity and specificity were 0.928, 93.3%, 91.7% and 0.658, 73.3%, 58.3% for two diagnosis methods respectively. The result showed significant difference between two methods with P = 0.002 (Table 5, Figure 3).Discussion
In this study, rFOV IRIS-DWI sequence significantly improved the diagnosis performance for T staging of rectal cancer patients. Compared with conventional single-shot EPI (ssEPI) DWI sequence, IRIS-DWI sequence used multiple excitations and two-dimensional navigation echo pulse technology. The technology can detect the phase changes introduced by intestinal motion between different multiple excited K-space subsets. Previous studies showed that IRIS-DWI may improve the image quality of the female pelvis7. And improved image quality could also be observed for the rectum. The rFOV IRIS-DWI may help us evaluate the relation between the tumor and normal tissue of the intestinal. So, rFOV IRIS-DWI significantly improved the diagnosis performance in rectal cancer T staging.Conclusion
rFOV IRIS-DWI combined T2WI imaging could provide higher diagnosis confidence and higher diagnosis accuracy for rectal cancer T staging.Fund programs
Jiangsu Medical Association Roentgen Imaging Research Fund (No.SYH-3201150-0013); Jiangsu Traditional Chinese Medicine Science and Technology Development Program (MS2021100); Key Research and Development Program of Xuzhou Science and Technology Bureau (KC20159); Aged Health Research Project of Jiangsu Provincial Health Commission (LKM2022018)Acknowledgements
No acknowledgement found.References
1. Krdzalic, J.; Maas, M.; Gollub, M. J.; Beets-Tan, R. G. H., Guidelines for MR imaging in rectal cancer: Europe versus United States. Abdom Radiol (NY) 2019, 44 (11), 3498-3507.
2. Beets-Tan, R. G. H.; Lambregts, D. M. J.; Maas, M.; Bipat, S.; Barbaro, B.; Curvo-Semedo, L.; Fenlon, H. M.; Gollub, M. J.; Gourtsoyianni, S.; Halligan, S.; Hoeffel, C.; Kim, S. H.; Laghi, A.; Maier, A.; Rafaelsen, S. R.; Stoker, J.; Taylor, S. A.; Torkzad, M. R.; Blomqvist, L., Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 2018, 28 (4), 1465-1475.
3. Gollub, M. J.; Arya, S.; Beets-Tan, R. G.; dePrisco, G.; Gonen, M.; Jhaveri, K.; Kassam, Z.; Kaur, H.; Kim, D.; Knezevic, A.; Korngold, E.; Lall, C.; Lalwani, N.; Blair Macdonald, D.; Moreno, C.; Nougaret, S.; Pickhardt, P.; Sheedy, S.; Harisinghani, M., Use of magnetic resonance imaging in rectal cancer patients: Society of Abdominal Radiology (SAR) rectal cancer disease-focused panel (DFP) recommendations 2017. Abdom Radiol (NY) 2018, 43 (11), 2893-2902.
4. Bates, D. D. B.; Homsi, M. E.; Chang, K. J.; Lalwani, N.; Horvat, N.; Sheedy, S. P., MRI for Rectal Cancer: Staging, mrCRM, EMVI, Lymph Node Staging and Post-Treatment Response. Clin Colorectal Cancer 2022, 21 (1), 10-18.
5. Gollub, M. J.; Lall, C.; Lalwani, N.; Rosenthal, M. H., Current controversy, confusion, and imprecision in the use and interpretation of rectal MRI. Abdominal Radiology 2019, 44 (11), 3549-3558.
6. Nougaret, S.; Jhaveri, K.; Kassam, Z.; Lall, C.; Kim, D. H., Rectal cancer MR staging: pearls and pitfalls at baseline examination. Abdominal Radiology 2019, 44 (11), 3536-3548. 7. An, H.; Ma, X.; Pan, Z.; Guo, H.; Lee, E. Y. P., Qualitative and quantitative comparison of image quality between single-shot echo-planar and interleaved multi-shot echo-planar diffusion-weighted imaging in female pelvis. Eur Radiol 2020, 30 (4), 1876-1884.
Figures