1448
Whole-Body Diffusion-weighted MRI, non-diffusion MRI, and PET-CT in detection of Spinal Lesions in Multiple Myeloma Patients1Department of Radiology, Peking University Third Hospital, Beijing, China, 2Peking University Third Hospital, Beijing, China, 3MR Collaboration, Siemens Healthineers Ltd, Beijing, China
Synopsis
Keywords: Bone, Diffusion/other diffusion imaging techniques, Multiple Myeloma
This study investigated the performance of whole-body diffusion-weighted imaging (WBDWI), non-diffusion MRI, and 18F-FDG PET-CT in detecting spinal lesions in patients with an initial diagnosis of multiple myeloma (MM). The results showed that WBDWI discovered more lesions compared with both non-diffusion MRI and 18F-PET-CT. And the detection of spinal lesions in WBDWI was not significantly decreased even with the decreased degree of marrow infiltration in patients with MM. This suggests that WBDWI should be the preferentially recommended examination for patients with an initial diagnosis of MM.Introduction
Multiple myeloma (MM) is the second most common hematological malignancy. There have been a lot of new therapies for MM with different indications. Radiology plays an important role in providing a sensitive and accurate evaluation of the treatment effect. At present, non-diffusion MRI and 18F-FDG PET-CT are recommended as the preferred methods for diagnosis and prognostic analysis of MM by the guideline [1]. PET-CT is superior to non-diffusion MRI for tumor activity analysis and therapy evaluation, but involves radiation and is more expensive [2]. Whole-body diffusion-weighted imaging (WBDWI) was first proposed in 2004. It has shown great potential in the diagnosis, therapy evaluation, and prognosis analysis of tumors with high sensitivity, no radiation, and easy quantitative analysis [3-4]. Nowadays, few studies have compared the performances of WBDWI, non-diffusion MRI, and 18F-FDG PET-CT in detecting spinal lesions in patients with an initial diagnosis of MM. Therefore, the main purpose of this study was to compare the efficacy of WBDWI, non-diffusion MRI, and 18F-FDG PET-CT in the detection of spinal lesions in patients with an initial diagnosis of MM, and to analyze the correlation between the detection of diffuse lesions and clinical data.Methods
Twenty-six patients with an initial diagnosis of MM who had undergone WBDWI, non-diffusion MRI, and PET-CT were retrospectively analyzed. WBDWI and non-diffusion MRI were acquired on a 3T MR scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany). Non-diffusion MRI included sagittal T1 weighted imaging (T1w) and axial T2 weighted short T1 inversion recovery (T2w STIR) sequence. WBDWI was performed with five consecutive positions in the axial direction using the EPI-DWI sequence. Scanning parameters for non-diffusion MRI and WBDWI and were as follows: T1w TSE, TR 400 ms, TE 8.8 ms, FOV=380×380 mm², slice thickness 4.0 mm, 15 slices; T2w STIR, TR 8190 ms, TE 57.0 ms, FOV=380×380 mm², slice thickness 5.0 mm,50 slices; DWI, TR 6480 ms, TE 63.0 ms, FOV= 450×450 mm², slice thickness 6.0 mm,40 slices,b values of 50 and 800s/mm2. The total acquisition times were 26 to 30 mins. PET-CT images were acquired on Siemens Biograph 64 PET-CT (Siemens Healthcare, Forchheim, Germany). Spinal lesions detected by the three imaging methods were scored. The gold standard was followed the guideline of MY-RADS in the reference [5]. The difference in the number of diseased vertebrae detected was also compared. In addition, the difference in clinical data between the diffuse infiltration group and the non-diffuse infiltration group for the three methods was assessed.Results
Scores were higher for WBDWI than for non-diffusion MRI and PET-CT in the whole and each region of the spine (P<0.05). The total number of diseased vertebrae detected in WBDWI (24.9) was higher than in non-diffusion MRI (21.7) and PET-CT (21) (P<0.05). For PET-CT, M protein and proportion of abnormal bone marrow plasma cells were both significantly higher in the diffuse infiltration group than in the non-diffuse infiltration group (P<0.05), but no difference between different groups of both WBDWI and non-diffusion MRI (P>0.05).Discussion
This was a preliminary study comparing the differences between WBDWI, non-diffusion MRI, and 18F-FDG PET-CT in the detection of spinal lesions in patients with an initial diagnosis of MM. We found that WBDWI can discover more spinal lesions compared with non-diffusion MRI and PET-CT in the cervical vertebra, thoracic vertebra, lumbar vertebra, or sacrum and coccyx. And the detection of spinal lesions in WBDWI and non-diffusion MRI would not be significantly influenced by the degree of marrow infiltration in patients of MM.Conclusion
Compared to non-diffusion MRI and 18F-FDG PET-CT, WBDWI has a higher sensitivity for spinal lesion detection in patients with an initial diagnosis of MM, and the sensitivity of lesion detection in WBDWI will not decrease with a low degree of marrow infiltration. Therefore, WBDWI seems to be more suited to be recommended as the preferred imaging examination in patients with an initial diagnosis of MM.Acknowledgements
No acknowledgement found.References
[1] HILLENGASS J, USMANI S, RAJKUMAR SV, et al. International myeloma working group consensus recommendations on imaging in monoclonal plasma cell disorders[J]. Lancet Oncol. 2019. 20(6): e302-e312. DOI: 10.1016/S1470-2045(19)30309-2.
[2] ZAMAGNI E, TACCHETTI P, CAVO M. Imaging in multiple myeloma: How? When[J]. Blood. 2019. 133(7): 644-651. DOI: 10.1182/blood-2018-08-825356.
[3] MESGUICH C, LATRABE V, HULIN C, et al. Prospective Comparison of 18-FDG PET/CT and Whole-Body MRI with Diffusion-Weighted Imaging in the Evaluation of Treatment Response of Multiple Myeloma Patients Eligible for Autologous Stem Cell Transplant[J]. Cancers (Basel). 2021. 13(8): 1938. DOI: 10.3390/cancers13081938.
[4] CHEN J, LI C, TIAN Y, et al. Comparison of Whole-Body DWI and 18F-FDG PET/CT for Detecting Intramedullary and Extramedullary Lesions in Multiple Myeloma[J]. AJR Am J Roentgenol. 2019. 213(3): 514-523. DOI: 10.2214/AJR.18.20989.
[5] MESSIOU C, HILLENGASS J, DELORME S, et al. Guidelines for Acquisition, Interpretation, and Reporting of Whole-Body MRI in Myeloma: Myeloma Response Assessment and Diagnosis System (MY-RADS) [J]. Radiology. 2019. 291(1): 5-13.
Figures
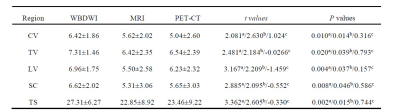
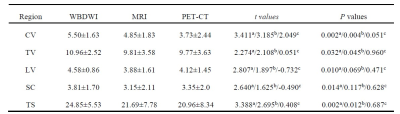
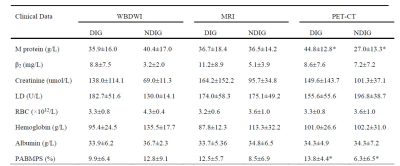
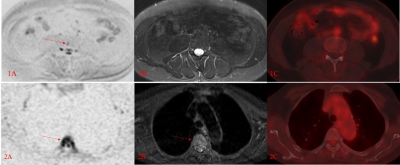
Figure 1 Representative images from two patients with multiple myeloma (MM).
1A)~1C) 55/M, focal lesion in the third lumbar vertebra with the size of 8.8×6.7mm. This lesion was discovered in 1A) WBDWI, but not in 1B) T2 STIR and 1C) PET.
2A)~2C) 67/F, diffuse lesions in the fourth thoracic with the proportion of abnormal bone marrow plasma cells of 2.21%, lesions were discovered in 2A) WBDWI and 2B) T2 STIR, but not diagnosed in 2C) PET.