1440
Flexural Rigidity of THAs is Associated with MRI and Histological findings
Sara E Sacher1, Elexis Padgett1, John P Neri1, Timothy Wright1, Thomas W Bauer1, Michael Parides1, Douglas Padgett1, Hollis G Potter1, and Matthew F Koff1
1Hospital for Special Surgery, New York, NY, United States
1Hospital for Special Surgery, New York, NY, United States
Synopsis
Keywords: MSK, MSK, Total hip arthroplasty
Micromotion at interfaces in modular total hip arthroplasties (THAs) induces corrosion and generation of adverse local tissue reactions (ALTRs), potentially leading to premature failure. The flexural rigidities (FR) of THA femoral stem trunnions retrieved from revision surgery were correlated with MRI metrics and histopathological outcomes. Increased FR was associated with osteolysis and a reduced synovial response, while a lower FR was associated with granulomas, different synovitis types, and tissue necrosis. These results indicate that MRI can serve as a useful biomarker of the local tissue response around THA.Introduction
Modular connections at the head-neck junction in total hip arthroplasty (THA) provide intraoperative choice but can contribute to corrosion and wear debris1,2. The debris can lead to adverse local tissue reactions (ALTRs) in the surrounding soft tissues leading to premature failure3. Previous work primarily focused on the evaluation of metal-on-metal (MOM) THA or hip resurfacing arthroplasty (HRA) designs4, but more traditional THA designs such as metal-on-polyethylene (MOP) and ceramic-on-polyethylene (COP) bearing surfaces have also been associated with the development of ALTRs4,5. Flexural rigidity (FR), a measure of the stiffness of a structure as a result of material composition and geometry, is a risk factor for corrosion due to its effect on interfacial head-stem micromotion6. While previous studies reported a negative correlation between FR and the severity of implant corrosion and fretting1,7, none examined the relationship between FR and clinical imaging outcomes. Magnetic resonance imaging (MRI) and histopathology have been used to identify and characterize ALTRs8, but how MRI outcomes relate to FR of failed THAs is unknown. Therefore, the objective of this study was to determine if differing implant FR’s are associated with unique MRI imaging metrics and histopathological outcomes.Methods
This study had IRB approval and informed written consent was obtained. The types of THAs meeting inclusion were MOM, MOP, COP, and ceramic-on-ceramic (COC). 320 patients undergoing revision THA surgery were sequentially recruited for whom complete data were available for 84. MRIs were obtained prior to revision surgery using clinical 1.5T scanners with an 8-channel phased array cardiac coil. 2D-FSE images were acquired in the axial, sagittal, and coronal planes9; coronal 3D MAVRIC-SL and MAVRIC-SL STIR images10 were also acquired. MR images were evaluated for the presence (y/n) and type of synovitis (fluid, solid, mixed), impression of synovium (normal, ALTR, infection, metallosis, polymeric, or abnormal), synovial thickness, ALTR severity (none, mild, moderate, severe), and presence (y/n) and location of osteolysis (femoral/acetabular)8. Tissue samples at the inferomedial aspect of the head-neck junction were acquired during revision surgery and the histologic findings were scored using Campbell’s aseptic lymphocyte-dominated vasculitis-associated lesion (ALVAL) score11 and the Natu12 and Fujishiro13 grading methods, which semi-quantitatively evaluate the presence of histiocytes, tissue particles, inflammation, and necrosis. Retrieved femoral stems underwent 3D laser scanning (Creaform, HandyScan), and Geomagic software (Morrisville, NC, USA) was used to extract geometric properties from the scans to calculate the FR of the trunnion as: $$ Flexural Rigidity = Ey * π * \frac{(Engagement Diameter)^4} {64} $$, where EY is the elastic modulus of the material and the engagement diameter is measured at the distal end of the male taper (Fig. 1). Regression models were used to determine relationships between variables of interest and flexural rigidity, controlling for age, BMI, sex, and length of implantation (SAS V.9.3). Statistical significance was set at p<0.05.Results
The mean FR of the 84 retrieved stems was 228 Nm2, with the most flexible and rigid stems having FRs of 87 Nm2 and 489 Nm2, respectively. FR was associated with the presence of osteolysis on MRI, synovitis type, granuloma presence, and necrosis severity (Fig. 2). Increased FR was also associated in individuals with geographic osteolysis on MRI (+55 Nm2, p = 0.038) compared to those without. When evaluated by region, the presence of femoral osteolysis was associated with higher FR (+62 Nm2, p = 0.022) and the presence of periacetabular osteolysis was associated with higher FR (+64 Nm2, p = 0.018). Further, FR was lower for subjects with fluid synovitis (-166 Nm2, p = 0.0026) or mixed synovitis (-119 Nm2, p = 0.020) as compared to subjects with no synovitis present on MRI. Lower FR was observed in individuals with granuloma (-88 Nm2, p = 0.030). Finally, individuals with the most severe grading of necrosis (grade 4) had stems with lower FR compared to those with the second most severe necrosis grading (grade 3) (-97 Nm2, p = 0.038).Discussion
In this study of patients undergoing revision THA surgery, an increase of femoral trunnion FR was associated with the presence of osteolysis and a reduced synovial response while a lower FR was associated with the presence of granulomas, different synovitis types, and tissue necrosis. The association between decreased FR with the presence of granulomas and necrosis severity is aligned with previous findings that THAs with lower trunnion FR resulted in higher corrosion1,7. These results suggest that micromotion from more flexible trunnions may enhance adverse local tissue responses to corrosion. Similarly, the lower FR observed in individuals with synovitis present compared to those without could indicate an inflammatory response to particulate debris. The positive relationship between FR and osteolysis indicates that a highly rigid femoral stem trunnion could alter the natural strain distribution in the femoral and acetabular bones and subsequently alters the biomechanically induced bone remodeling process14, 15.Conclusion
The biologic impact of varying implant stiffness in THA manifests with differing MRI and histologic features, and imaging can serve as a useful biomarker of the local tissue response.Acknowledgements
Research reported in this abstract was supported by NIAMS/NIH under award number AR064840.References
1Kao et al, J Arthroplasty 2016; 2Esposito et al, Clin. Orthop. Relat. Res. 2014; 3Hannon et al, J. Arthroplasty 2020; 4Higgs et al, J. Arthroplasty 2013; 5Triantafyllopoulos et al, Clin. Orthop. Relat. Res. 2016; 6Haschke et al, Med. Eng. Phys. 2019; 7Goldberg et al, Clin. Orthop. Relat. Res. 2002; 8Koff et al, Clin. Orthop. Relat. Res. 2019; 9Hayter et al, J. Magn. Reson. Imaging 2012; 10Hayter et al, AJR 2011; 11Campbell et al, Clin. Orthop. Relat. Res, 2010; 12Natu et al, J. Clin. Pathol, 2011; 13Fujishiro et al, Clin. Orthop. Relat. Res., 2011; 14Ma et al, Orthopedics, 1997; 15Chatterjee et al, J. Biomech. Eng., 2020.Figures
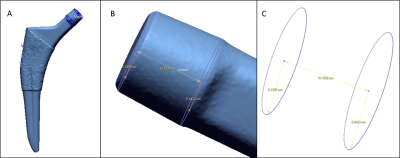
Figure
1. Representative 3D laser scan of a retrieved Trilock (Depuy) femoral stem.
(A) The full stem was scanned using a handheld 3D laser scanner (Creaform,
HandyScan). (B) From the laser scan, the proximal and distal radii of the
trunnion’s taper were determined using Sketch functions in Geomagic DesignX
software. The radii and the length of the trunnion’s taper were used to
calculate the flexural rigidity of the femoral stem.
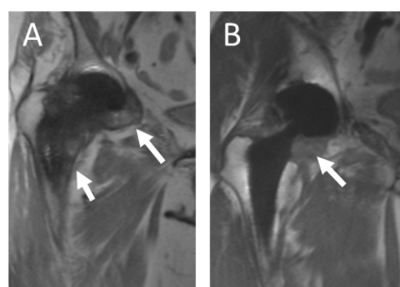
Figure
2. A) Coronal MAVRIC image of a patient with a MOP THA (81 F / Length of
implantation: 17.8 years) displaying periacetabular and femoral osteolysis
(arrows)) Coronal MAVRIC image of a MOP THA (56 M, Length of implantation: 0.58
years, FR=489.2 Nm2) demonstrating the synovial reaction of an ALTR (arrow).
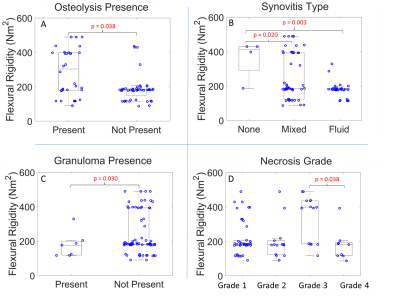
Figure
3. Flexural Rigidity varied with unique MRI and histopathological findings. A) A
higher FR is associated with the presence of osteolysis on MRI. B) A lower FR
is associated with the presence of mixed or fluid synovitis on MRI compared to
no synovitis. C) A lower FR is associated with the presence of granuloma. D) A
lower FR is associated with a more severe necrosis grading (grade 4) compared
to grade 3.
DOI: https://doi.org/10.58530/2023/1440