1408
Submillimeter morphologic lung MRI at 0.55T using balanced steady-state free precession with half-radial dual-echo readout (bSTAR)
Grzegorz Bauman1,2, Nam G Lee3, Ye Tian4, Oliver Bieri1,2, and Krishna S Nayak3,4
1Deparment of Radiology, Division of Radiological Physics, University of Basel Hospital, Basel, Switzerland, 2Department of Biomedical Engineering, University of Basel, Basel, Switzerland, 3Department of Biomedical Engineering, Viterbi School of Engineering, University of Southern California, Los Angeles, CA, United States, 4Ming Hsieh Department of Electrical and Computer Engineering, Viterbi School of Engineering, University of Southern California, Los Angeles, CA, United States
1Deparment of Radiology, Division of Radiological Physics, University of Basel Hospital, Basel, Switzerland, 2Department of Biomedical Engineering, University of Basel, Basel, Switzerland, 3Department of Biomedical Engineering, Viterbi School of Engineering, University of Southern California, Los Angeles, CA, United States, 4Ming Hsieh Department of Electrical and Computer Engineering, Viterbi School of Engineering, University of Southern California, Los Angeles, CA, United States
Synopsis
Keywords: Lung, Low-Field MRI, Morphology
In this work we explore the potential of free-breathing balanced steady-state free precession half-radial dual-echo imaging technique (bSTAR) for morphologic lung MRI in human subjects using high-performance 0.55T MR-scanner. The technique combines an efficient minimal-TR readout sampling with interleaved wobbling Archimedean spiral pole trajectories and retrospective respiratory self-gating. Lung imaging at 0.55T helped to markedly reduce off-resonance artifacts while providing an improved signal intensity and allowed for high-quality morphologic lung MRI at a submillimeter spatial resolution.
Introduction
Despite the continuous improvement in the MRI technology and image post-processing techniques, lung MRI remains difficult, and its clinical application limited due to the problems associated with physical properties of the lung. Large magnetic susceptibility differences at the microscopic scale of alveoli combined with the unfavorable relaxation times (long T1, short T2 and T2*) lead to rapid signal decay and are especially pronounced at standard clinical field strengths (>1.5T). Hence, in the recent years there has been a growing interest in exploring lung MRI on scanner configurations operating at lower field strengths with high performance gradient systems 1,2. Lower field strength helps to reduce susceptibility artifacts, off-resonance artifacts and provides more favorable relaxation times 3. One of the techniques that has shown to be well-suited for lung imaging is balanced steady-state free precession (bSSFP). It offers a unique T2/T1 contrast and highest signal-to-noise ratio (SNR) per time unit compared to incoherent SSFP techniques 4. Recently, a 3D half-radial dual-echo bSSFP technique known as bSTAR has been demonstrated to provide compelling results for morphologic lung imaging at 1.5T 5,6. In this work, we explore a free-breathing bSTAR technique for high-resolution morphologic lung MRI in human subjects at 0.55T.Methods
MR data acquisitionExperiments were performed using a whole-body 0.55T system (prototype MAGNETOM Aera, Siemens Healthineers, Erlangen, Germany) equipped with high-performance shielded gradients (45 mT/m amplitude, 200 T/m/s slew rate). Five healthy volunteers (mean age: 28.4 years, range: 25-39 years, three male, two female) were scanned with 3D bSTAR in the supine position during free-breathing. All subjects provided written informed consent, under a protocol approved by our Institutional Review Board.
MRI data were acquired using a 3D half-radial dual-echo bSTAR pulse sequence (Figure 1). The k-space data were sampled with an interleaved wobbling Archimedean spiral pole trajectory (5). The scans were performed with predefined shim settings and a combination of 6-channel body array and 12-elements of the table-integrated spine array for signal reception. Free breathing acquisitions were performed with field-of-view = 34x34x34 cm3, TE1/TE2/TR = 0.13/1.93/2.14 ms, 448 samples per half-radial projection, 200 us hard RF pulse, flip angle α = 20º, 1116 Hz/pixel bandwidth, 0.90 mm nominal isotropic resolution, 360,000 half-radial projections were acquired using 600 interleaves and resulted in scan time of 12:51 min.
Image reconstruction
bSTAR datasets were reconstructed off-line using compressed sensing with fast iterative shrinkage-thresholding algorithm (FISTA) (6). The datasets were reconstructed on a 5123 matrix with a k-space zoom factor of 0.73 resulting in 0.90 mm isotropic resolution matching the spatial resolution measured in k-space. K-space data acquired from both echoes was reconstructed separately and combined by a pixel-wise complex-valued addition. Signal modulation in the k-space center was used to detect respiratory phase, as described previously (7). The respiratory signal modulation picked up by the anterior and posterior coils was extracted using randomized singular value decomposition. Readouts acquired during the end-expiratory phase were binned and used for reconstructions of separate 3D volumes. The reconstruction pipeline was written in C++ with CUDA Toolkit 11.7 (NVIDIA Corp. Santa Clara, CA) on a workstation equipped with Quadro P6000 GPU (NVIDIA Corp.).
Results
Figure 2 shows exemplary bSTAR reconstructions from two healthy volunteers in coronal, sagittal and axial views. The submillimeter spatial resolution allows for visualization up to the eight generation of vessels and fifth generation of bronchi. Furthermore, a gravity-related signal intensity distribution can be noticed on sagittal and axial views. Maximum intensity projection images for improved visualization of pulmonary vasculature reconstructed from the bSTAR datasets are shown in Figure 3. No noticeable off-resonance artifacts or ghosting due to the pulsatile heart motion can be observed on the images. Figure 4 shows an animation of a reconstructed bSTAR dataset in axial view.Discussion and Conclusion
In this work, we demonstrated the feasibility of free-breathing 3D bSTAR lung imaging with respiratory self-gating in healthy subjects on a high-performance 0.55T MR-system. The bSTAR technique profits from maximal sampling efficiency (~85% of TR) as well as from a high intrinsic SNR offered by the bSSFP signal. Data acquisition at 0.55T helped to successfully mitigate off-resonance artifacts in the whole field-of-view. The combination of the aforementioned beneficial factors allows for artifact-free imaging with a submillimeter isotropic spatial resolution. Future studies will focus on the exploration of the clinical added value of the free-breathing bSTAR technique in patients with pulmonary disease.Acknowledgements
We acknowledge grant support from the National Science Foundation (#1828736) and research support from Siemens Healthineers.References
- Campbell-Washburn AE, Malayeri AA, Jones EC et al. T2-weighted Lung Imaging Using a 0.55-T MRI System. Radiol Cardiothorac Imaging. 2021 Jun 10;3(3):e200611.
- Javed A, Ramasawmy R, O'Brien K et al. Self-gated 3D stack-of-spirals UTE pulmonary imaging at 0.55T. Magn Reson Med. 2022 Apr;87(4):1784-1798.
- Li B, Lee NG, Cu SXi, Nayak KS. Lung parenchyma transverse relaxation rates at 0.55 Tesla. Magn Reson Med. accepted.
- Scheffler K, Lehnhardt S. Principles and applications of balanced SSFP techniques. Eur Radiol. 2003;13:2409–2418.
- Bauman G, Bieri O. Balanced steady-state free precession thoracic imaging with half-radial dual-echo readout on smoothly interleaved archimedean spirals. Magn Reson Med. 2020 Jul;84(1):237-246.
- Bieri O, Pusterla O, Bauman G. Free-breathing half-radial dual-echo balanced steady-state free precession thoracic imaging with wobbling Archimedean spiral pole trajectories. Z Med Phys. 2022 Feb 18:S0939-3889(22)00003-4.
- Beck A, Teboulle M. A fast iterative shrinkage-thresholding algorithm for linear inverse problems. SIAM J Imaging Sci. 2009;2:183–202.
- Larson AC, White RD, Laub G et al. Self-gated cardiac cine MRI. Magn Reson Med 2004;51:93–102.
Figures
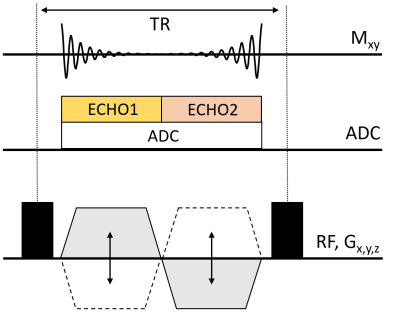
Figure 1. Pulse sequence diagram for bSTAR imaging with
half-radial dual-echo readout along the bipolar gradients Gx, Gy, Gz and a
non-selective RF pulse excitation. Consequently, the k-space is sampled with
both center-out and center-in half-radial projections. One single ADC is used
that spans along the full free precession period for maximum sequence
efficiency.
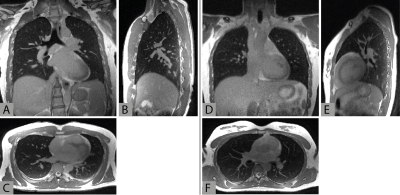
Figure 2. Illustrative
thorax images obtained with free-breathing bSTAR in two different
volunteers (left: volunteer
#1 - 39 year old male, right: volunteer #5 - 27 year old female). The
datasets were reconstructed at 0.9 mm isotropic resolution in coronal (A,D),
sagittal (B,E) and axial (C,F) views.
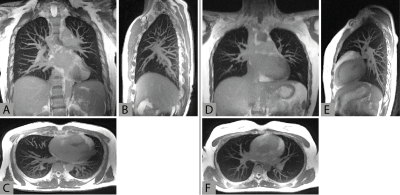
Figure 3. Maximum
intensity projection (MIP) images reconstructed with 15 mm thickness in coronal
(A,D), sagittal (B,E) and axial (C,F) views from the datasets presented in
Figure 2.

Figure 4. Animation showing coronal reconstruction with 0.9 mm isotropic spatial resolution obtained using free-breathing bSTAR in volunteer #1.
DOI: https://doi.org/10.58530/2023/1408