1404
UTE-MRI with Single- and Dual-Echo Methods vs. CT: Differentiation Capability of Non- or Minimally Invasive Adenocarcinomas from Other Cancers1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Fujita Health University School of Medicine, Toyoake, Japan, 5Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan, 6Fujita Health University Hospital, Toyoake, Japan
Synopsis
Keywords: Lung, Cancer
We hypothesized that pulmonary MRIs with UTE using single- or dual-echo techniques may be equal to or more useful than standard-dose thin-section CT for evaluating solid portion size and C/T ratio. The purpose of this study was thus to compare capabilities of pulmonary MRIs with UTE using single- and dual-echo techniques (UTE-MRISingle and UTE-MRIDual) and thin-section CT for quantitative differentiation of non- and minimally invasive adenocarcinomas from other lung cancers.Introduction
The results of a multicenter, open-label, phase 3, randomized, controlled and non-inferiority trial to compare segmentectomy and lobectomy for small-sized peripheral non-small-cell lung cancer (NSCLC) were reported in 2022 (1). Moreover, it has been suggested that radiological determination of invasiveness for lung adenocarcinoma on thin-section CT can be useful for patient management as well as outcome, and that the consolidation/tumor (C/T) ratio on thin-section CT may be an effective predictor in these settings (1-5). Since the 2010s, the use of pulmonary MRIs with an ultra-short TE (UTE) has been recommended as useful for morphological and physical evaluations of lung parenchyma abnormalities and may be able to function as a substitute for thin-section standard-dose or low-dose CTs for radiological finding evaluation, nodule detection and evaluation, lung cancer screening or Lung Imaging Reporting and Data System (Lung-RADS) classification (6-8). In addition, Canon Medical Systems Corporation has recently provided for clinical use a new pulmonary MRI with UTE using the dual-echo technique, which makes it possible to obtain MR images with two different UTEs for morphological change evaluation. However, no direct comparisons have been performed among pulmonary MRIs with UTE with single- and dual-echo techniques, standard-dose CT and pathological examination results for evaluating solid portion size and C/T ratio. Moreover, no study published in the literature has clearly established the utility of pulmonary MRI with UTE using the dual-echo technique as compared with that of using the single-echo technique for the same setting. We hypothesized that pulmonary MRIs with UTE using single- or dual-echo techniques may be equal to or more useful than standard-dose thin-section CT for evaluating solid portion size and C/T ratio. The purpose of this study was thus to compare capabilities of pulmonary MRIs with UTE using single- and dual-echo techniques (UTE-MRISingle and UTE-MRIDual) and thin-section CT for quantitative differentiation of non- and minimally invasive adenocarcinomas (MIA) from other lung cancers in stage IA lung cancer patients.Materials and Methods
Ninety pathologically diagnosed stage IA lung cancer patients who underwent thin-section standard-dose CT, UTE-MRISingle and UTE-MRIDual, surgical treatment and pathological examinations were included in this study. All patients underwent thin-section standard-dose CT examinations with automatic exposure control with an image SD of 15 on three 320-detector row CT scanners (Aquilion ONE; Canon Medical Systems Corporation, Otawara, Tochigi, Japan). Moreover, pulmonary MRIs with UTE were performed with the aid of a respiratory-gated three-dimensional (3D) radial UTE pulse sequence with single-echo (UTE-MRISingle : TR 3.7 ms/ TE 0.096 ms, flip angle: 5°, voxel size: 1×1×1 mm3) and dual-echo (UTE-MRIDual : TR 8.1 ms/ TE 0.096 and 2.3 ms, flip angle: 5°, voxel size: 1×1×1 mm3) techniques in the coronal plane with two 3 T MRI systems (Vantage Centurian: Canon Medical Systems) using a 16-element phased-array body coil and a 16-element phased-array spine coil combined with parallel imaging capability. All pulmonary MRIs obtained with UTE were then reconstructed as 1 mm-thick sections in the axial and coronal planes. Then, the largest dimension (Dlong), solid portion (solid Dlong) and consolidation/tumor (C/T) ratio of each nodule were assessed by UTE-MRISingle, 1st and 2nd echo on UTE-MRIDual (UTE-MRIDual1st echo and UTE-MRIDual2nd echo) and lung or mediastinal window settings on CT (CTLung and CTMediastinal). To determine the relationships of Dlong, solid Dlong and C/T ratio with each method and pathological examination result, correlations and the limits of agreement for Dlong, solid Dlong and C/T ratio were evaluated by means of Pearson’s correlation and the Bland-Altman method for all MRI methods and CTMediastinal. Then, Receiver operating characteristic (ROC)-based positive tests were performed to determine all feasible threshold values of Dlong, solid Dlong and C/T ratio obtained with each method for differentiating non- and minimally invasive adenocarcinomas such as adenocarcinoma in situ (AIS) and minimally invasive adenocarcinoma (MIA) from other lung cancers. Finally, McNemar’s test was used to compare sensitivity, specificity and accuracy of each of the methods. A p-value less than 0.05 was considered significant for all statistical analyses.Results
Representative cases are shown in Figure 1. Correlations and the limits of agreement for Dlong, solid Dlong and C/T ratio measurements between obtained with each method and from pathological examination result are shown in Figure 2. Correlations ranged from significant to excellent between each of the methods and pathological examination results for all indexes except C/T ratio on CTMediastinal (0.95≤r≤0.99, p<0.0001). Moreover, the C/T ratio for CTMediastinal showed from good to significant with pathological examination results (r=0.88, p<0.0001). The limits of agreement for Dlong and solid Dlong and C/T ratio with pathological examination results for all methods were determined as small enough for clinical purpose. Results of a comparison of diagnostic performance by all indexes are shown in Figure 3. Specificities and accuracies of solid Dlong and C/T ratio were significantly higher than those of Dlong for each of the methods (p<0.05). Moreover, specificities and accuracies of solid Dlong for UTE-MRIDual2nd echo and CTMediastinal were significantly higher than those of solid Dlong for UTE-MRISingle and UTE-MRIDual1st echo, and C/T ratio on all methods except CTMediastinal (p<0.05).Conclusion
MRI with UTE’s capability for quantitative differentiation of non- and minimally invasive adenocarcinomas from other lung cancers is equal or superior to that of thin-section CT.Acknowledgements
This study was technically and financially supported by Canon Medical Systems Corporation.References
- Saji H, Okada M, Tsuboi M, et al; West Japan Oncology Group and Japan Clinical Oncology Group. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022;399(10335):1607-1617.
- Suzuki K, Koike T, Asakawa T, et al; Japan Lung Cancer Surgical Study Group (JCOG LCSSG). A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol. 2011 Apr;6(4):751-756.
- Asamura H, Hishida T, Suzuki K, et al; Japan Clinical Oncology Group Lung Cancer Surgical Study Group. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg. 2013;146(1):24-30.
- Suzuki K, Watanabe S, Mizusawa J, et al; Japan Lung Cancer Surgical Study Group (JCOG LCSSG). Predictors of non-neoplastic lesions in lung tumours showing ground-glass opacity on thin-section computed tomography based on a multi-institutional prospective study†. Interact Cardiovasc Thorac Surg. 2015;21(2):218-223. doi: 10.1093/icvts/ivv124.
- Kanamoto Y, Sakao Y, Kuroda H, et al. Selection of Pathological N0 (pN0) in Clinical IA (cIA) Lung Adenocarcinoma by Imaging Findings of the Main Tumor. Ann Thorac Cardiovasc Surg. 2021;27(4):230-236.
- Ohno Y, Koyama H, Yoshikawa T, et al. Pulmonary high-resolution ultrashort TE MR imaging: Comparison with thin-section standard- and low-dose computed tomography for the assessment of pulmonary parenchyma diseases. J Magn Reson Imaging. 2016;43(2):512-532.
- Ohno Y, Koyama H, Yoshikawa T, et al. Standard-, Reduced-, and No-Dose Thin-Section Radiologic Examinations: Comparison of Capability for Nodule Detection and Nodule Type Assessment in Patients Suspected of Having Pulmonary Nodules. Radiology. 2017;284(2):562-573.
- Wielpütz MO, Lee HY, Koyama H, et al. Morphologic Characterization of Pulmonary Nodules With Ultrashort TE MRI at 3T. AJR Am J Roentgenol. 2018;210(6):1216-1225.
Figures
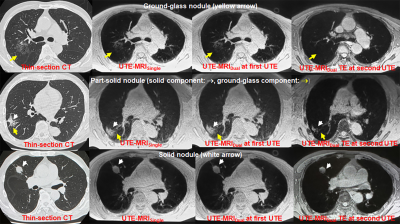
Figure 1. Thin-section CT and all UTE-MRIs in patients with ground-glass nodule (GGN), part-solid nodule and solid nodule.
Thin-section CT, UTE-MRISingle, UTE-MRIDual1st echo and UTE-MRIDual 2nd echo shows ground-glass nodule (GGN), part-solid nodule and solid nodule . CT, UTE-MRISingle and UTE-MRIDual1st echo clearly demonstrate all types of nodules. UTE-MRIDual2nd echo can not be demonstrate GGN as well as GGO within part-solid nodule (yellow arrows), although it can accurately demonstrate solid component within part-solid nodule as well as solid nodule (white arrows).
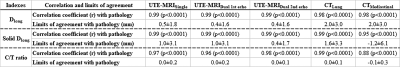
Figure 2. Correlations and the limits of agreement for Dlong, solid Dlong and C/T ratio measurements between obtained with each method and from pathological examination result.
Correlations ranged from significant to excellent between each of the methods and pathological examination results for all indexes except C/T ratio on CTMediastinal (0.95≤r≤0.99, p<0.0001), although the C/T ratio for CTMediastinal showed good correlation (r=0.88, p<0.0001). The limits of agreement for all indexes were determined as small enough for clinical purpose.
