1398
UTILITY OF OXYGEN-ENHANCED LUNG MRI IN LONG TERM POST-LUNG TRANSPLANT PATIENT CARE1Department of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3Department of Respiratory Medicine, Hannover Medical School, Hannover, Germany
Synopsis
Keywords: Lung, Transplantation, Graft loss
Aim of this prospective single-center surveillance study was to assess the ability of oxygen-enhanced MRI to predict future chronic lung allograft dysfunction (CLAD) related transplant loss. Baseline MRI scans were acquired 6-12 months and follow-up MRI 2.5 years after double lung transplantation. T1 mapping was carried out with patients breathing room air and 100% oxygen, Delta T1 maps were calculated. Median, quartile coefficient of dispersion and ventilated volume parameters were correlated with graft loss and compared with same day lung function testing. Oxygen-enhanced MRI predicted future CLAD-related transplant loss 6-12 months post transplantation and, when evaluating %change, at follow-up MRI.
INTRODUCTION
Chronic lung allograft dysfunction (CLAD) with related graft loss is one of the main long-term complications for lung transplant patients1. The clinical diagnosis of CLAD relies on spirometry. However, CLAD is often detected at a late stage of disease. Moreover, there is still no generally accepted biomarker to predict the development of CLAD-related re-transplantation or death2. While oxygen-enhanced MRI mapping parameters could detect bronchiolitis obliterans syndrome (an obstructive subtype of CLAD) in a cross-sectional single-center study3, this study’s aim was to assess the prognostic value of oxygen-enhanced MRI mapping biomarkers in predicting graft loss defined as re-transplantation or death due to CLAD in a longitudinal prospective single-center trial.METHODS
From June 2013 to December 2018, MRI scans of 141 double lung transplant recipients (65 female, age range 18-66) were acquired 6-12 months (baseline) and 2.5 years after transplantation (follow-up). The median total observation period was 6.1 years. Spirometry was performed on the same day. Coronal T1 maps of the lungs were acquired with the patient breathing room air and after application of 100% oxygen for 6 minutes via a closed face mask by using a Look-Locker inversion-recovery snapshot fast low-angle shot (FLASH) sequence3,4,5 at 1.5 T (MAGNETOM Avanto, Siemens Healthcare, Erlangen, Germany). A pair of FLASH sequences was taken while holding breath for about 7 seconds for each slice, registered and cross-correlated with each other. Room air maps were also cross-correlated with oxygen maps. Delta T1 maps were calculated by subtraction (T1room air –T1100% oxygen). For image analysis, lung parenchyma was segmented semiautomatically (see fig. 1). The Delta T1 maps’ respective median, quartile coefficient of dispersion (QCD, as a marker of heterogeneity), and ventilated volume (VV, the proportion of voxels above a threshold suggested by Jobst et al.6) inside the lung parenchyma were assessed. Clinical and MRI parameters were compared regarding CLAD-related graft loss (re-do transplant or death) as primary endpoint using Wilcoxon tests (α=0.05), Receiver operating characteristics (ROC), Kaplan-Meyer survival analysis and Cox proportional hazards model.RESULTS
At baseline MRI, 131 clinically stable patients were included, of which 24 patients had CLAD-related graft loss. While group comparisons of baseline MRI parameters did not show any significant difference between patients who did and who did not develop CLAD-related graft loss (Delta T1: median P=0.76, QCD P=0.88, VV P=0.60), the survival analysis showed that a change of the Delta T1 maps predicted a poorer survival:- Delta T1 median [msec] (cutoff=93.3; Log-Rank P=0.02; hazard ratio (HR) for graft loss 3.5, 95%CI 1.01-9.40, P=0.048, see fig. 2A),
- Delta T1 QCD (cutoff=0.49, Log-Rank P=0.01; HR for graft loss 3.43, 95%CI 1.12-8.70, P=0.03), and
- Delta T1 VV [%] values (cutoff=79.3, Log-Rank P=0.01; HR for graft loss 3.07, 95%CI 1.18-7.22, P=0.02, see fig. 2B)
Evaluating the follow-up MRI (102 patients, 11 of them reached the endpoint of CLAD-related graft loss), group comparisons using Wilcoxon tests showed significant differences: A reduction of Delta T1 median [%change to baseline] over time was associated with developing CLAD-related graft loss (P=0.048, 90.8 (62.7-106.9) vs. 103.6 (90.3-119.2)), whereas QCD and VV had no significant difference for CLAD-related graft loss (Delta T1: QCD P=0.40, VV P=0.19). Additionally,
survival analysis showed that also %change of Delta T1 maps predicted a poorer survival with higher hazard ratios (HR) compared to baseline analysis:
- Delta T1 median [%change to baseline] (cutoff=95.9, Log-Rank P=0.002; HR for graft loss 8.89, 95%CI 2.02-63.08, P=0.003, see fig. 2D),
- Delta T1 QCD [%change to baseline] (cutoff=132.7, Log-Rank P=0.003; HR for graft loss 6.34, 95%CI 1.49-27.03, P=0.01), and
- Delta T1 VV [%change to baseline] values (cutoff=91.4, Log-Rank P=0.002; HR for graft loss 6.94, 95%CI 1.63-29.49, P=0.01, see fig. 2E)
DISCUSSION
In this prospective longitudinal study with 141 participants, oxygen-enhanced T1 mapping predicted CLAD-related death or transplant loss in a large prospective post lung transplant cohort. At baseline, oxygen-enhanced MRI predicted future transplant loss due to chronic allograft dysfunction using the Delta of T1 values between room air and 100% oxygen (HR for graft loss 3.5), while spirometry did not.At follow-up, Delta T1 median [%change to baseline] (HR for graft loss 8.89), and forced expiratory volume in 1 second (FEV1 [%change to baseline], HR for graft loss 15.55) predicted future graft loss.
The MRI technique is patient friendly as it only requires the application of 100% oxygen for a short time during the MRI scan, which was well tolerated. Thus, oxygen-enhanced T1 mapping may add clinical value in monitoring patients post lung transplantation. The technology is ready to be further explored in a multicenter setting.
CONCLUSION
Oxygen-enhanced MRI biomarkers predict CLAD-related transplant loss or death in a large post lung transplant cohort and may add clinical value in monitoring post lung transplantation.Acknowledgements
This work was funded by the German Center for Lung Research (DZL).References
- Yusen RD, Edwards LB, Dipchand AI, Goldfarb SB, Kucheryavaya AY, Levvey BJ, Lund LH, Meiser B, Rossano JW, Stehlik J; International Society for Heart and Lung Transplantation. The Registry of the International Society for Heart and Lung Transplantation: Thirty-third Adult Lung and Heart-Lung Transplant Report-2016; Focus Theme: Primary Diagnostic Indications for Transplant. J Heart Lung Transplant. 2016 Oct;35(10):1170-1184.
- Verleden SE, Verleden GM. Novel biomarkers of chronic lung allograft dysfunction: is there anything reliable? Curr Opin Organ Transplant. 2022 Feb 1;27(1):1-6.
- Renne J, Lauermann P, Hinrichs JB, Schönfeld C, Sorrentino S, Gutberlet M, Jakob P, Haverich A, Warnecke G, Welte T, Wacker FK, Gottlieb J, Vogel-Claussen J. Chronic Lung Allograft Dysfunction: Oxygen-enhanced T1-Mapping MR Imaging of the Lung. Radiology. 2015 Jul;276(1):266-73.
- Nekolla S, Gneiting T, Syha J, Deichmann R, Haase A. T1 maps by K-space reduced snapshot-FLASH MRI. J Comput Assist Tomogr. 1992 Mar-Apr;16(2):327-32.
- Jakob PM, Hillenbrand CM, Wang T, Schultz G, Hahn D, Haase A. Rapid quantitative lung (1)H T(1) mapping. J Magn Reson Imaging. 2001 Dec;14(6):795-9.
- Jobst BJ, Triphan SM, Sedlaczek O, Anjorin A, Kauczor HU, Biederer J, Ley-Zaporozhan J, Ley S, Wielpütz MO. Functional lung MRI in chronic obstructive pulmonary disease: comparison of T1 mapping, oxygen-enhanced T1 mapping and dynamic contrast enhanced perfusion. PLoS One. 2015 Mar 30;10(3):e0121520.
Figures
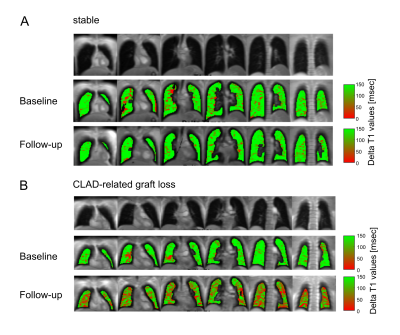
Figure 1: Exemplary coronal slices of oxygen-enhanced MRI. 1st row: morphology of the baseline examination. 2nd and 3rd row: Delta T1 mapping of baseline and follow-up. High T1 values are green, low values red. (A) Clinical stable patient (end of observation 42 months post follow-up). Ventilated Volume (VV) was stable from 93% on the day of baseline to 97% on follow-up 47 months later. (B) Patient with progressive CLAD (died 11 months post follow-up). VV declined from 95 to 75% after 24 months.
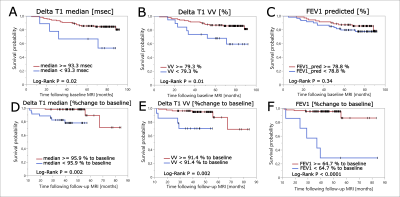
Figure 2: Survival by baseline (A-C) and follow-up (D-F) data visualized with Kaplan-Meyer plots. The respective cut-off values of Delta T1 median, ventilated volume (VV), and forced expiratory volume in 1 second (FEV1) to divide the population into subgroups (red and blue line) was calculated in the ROC analysis. The red graph represents the subgroup with better survival than the subgroup of the blue graph. Vertical lines along the graphs mark censored data.