1346
Carotid plaque predicts progression of intracranial atherosclerosis: A MR imaging-based community cohort study
Miaoxin Yu1, Dandan Yang2, Runhua Zhang1, Yong Jiang1, Huiyu Qiao3, Xihai Zhao3, Gaifen Liu1, and Yongjun Wang1
1Department of Neurology, Beijing Tiantan Hospital, Beijing, China, 2Department of Radiology, Beijing Geriatric Hospital, Beijing, China, 3Tsinghua University, Beijing, China
1Department of Neurology, Beijing Tiantan Hospital, Beijing, China, 2Department of Radiology, Beijing Geriatric Hospital, Beijing, China, 3Tsinghua University, Beijing, China
Synopsis
Keywords: Head & Neck/ENT, Atherosclerosis
Intracranial atherosclerotic disease progression is associated with recurrent stroke risk. In the present study, we investigated the association between carotid plaque and intracranial atherosclerosis progression in stroke-free participants using MR vessel wall imaging. In 312 participants recruited from a community cohort, we found that carotid plaque was independently associated with intracranial atherosclerosis progression during around 3-years’s follow-up. Our findings suggest that carotid plaque may be an effective predictor for intracranial atherosclerosis progression.Introduction
Intracranial atherosclerosis progression is associated with recurrent ischemic cerebrovascular events. 1 Hence, it is important to determine the influenced factors of intracranial atherosclerosis progression. Increasing evidence has shown that carotid and intracranial atherosclerosis share similar risk factors. 2 However, previous studies focused more on symptomatic intracranial atherosclerosis, 3 the association of carotid plaque with the progression of intracranial atherosclerosis in stroke-free participants is still unclear. This study aimed to investigate the association between carotid plaque and the progression of intracranial atherosclerosis in participants from a community cohort using MR vessel wall imaging.Methods
Study population: A total of 312 asymptomatic participants (mean age 59.85 ± 13.04 years; 136 males) were included from a community cohort in this study. The Institutional Review Board approved this study, and all participants provided written informed consent. MR imaging: All participants underwent carotid and intracranial artery MR vessel wall imaging on a 3T MR scanner (Philips Achieva TX, Philips Healthcare, Best, The Netherlands) using a custom-designed 36-channel neurovascular coil. For plaque evaluation, the following sequences were acquired: 3D T1-weighted volumetric isotropic turbo spin-echo acquisition (T1-VISTA) for intracranial plaque: turbo spin echo sequence; repetition time 800 ms; echo times 21 ms, field of view 20×18×4 cm3, and isotropic resolution 0.6 × 0.6 × 0.6 mm3; 3D motion-sensitized driven equilibrium prepared rapid gradient echo (MERGE) for carotid artery: fast field echo sequence; repetition time 8 ms, echo times 3.47 ms, flip angle 6°, field of view 20×16×4 cm3, and isotropic resolution 0.8 × 0.8 × 0.8 mm3. Follow-up study: All the recruited participants underwent a follow-up visit at 3.15 ± 0.59 years after the initial evaluation from July 2017 to September 2019. The follow-up MR imaging was performed using the same MR scanner and imaging protocol. Imaging analysis: Two observers with > 3 years' experience in neuroimaging blinded to the information of carotid and intracranial artery images from the same participant reviewed the MR images using a Digital Imaging and Communications in Medicine viewer (RadiAnt DICOM Viewer, Medixant, Poznan, Poland) with consensus. The presence, location, count, and burden (maximum wall thickness, length, and stenosis) of carotid and intracranial atherosclerotic plaques were evaluated. The progression of intracranial artery plaque was defined as the count of plaque increased, or the burden (length, maximum wall thickness, or stenosis) increased >20% between baseline and follow-up on 3D T1-VISTA images (Figure 1). Statistical analysis: Continuous data were compared using the independent t-test or Mann-Whitney U test. Categorical data were compared using the Chi-square test or Fisher exact test. The associations between baseline carotid plaque and the progression of intracranial atherosclerosis were analyzed using univariable and multivariable Cox regression, adjusted for age and sex (model 1), and history of smoke, hypertension, diabetes mellitus, antiplatelet medication, and HDL levels at baseline (model 2) which showed P < 0.05 in univariate analysis. SAS version 9.4 software (SAS Institute Inc., Cary, NC, USA) was used to analyze all data. A two-sided P value < 0.05 was considered as statistical significance.Results
Of the 312 participants, 85 (27.24%) had progression of intracranial atherosclerosis during follow-up. At least one carotid plaque was detected at baseline in 167 (53.53%) participants. In multivariable analyses, after adjusting for clinical confounders, presence of carotid plaque remained to be a significant predictor for the progression of intracranial atherosclerosis (Hazard ratio, 1.83; 95% confidence interval, 1.05-3.19, P = 0.033) (Table 1).Discussion and Conclusion
We found that carotid artery atherosclerotic plaque is an independent predictor for progression of intracranial atherosclerosis in the asymptomatic participants. Because the presence of carotid plaque can be well determined by ultrasound imaging which has better availability and cost effectiveness compared to MRI, evaluating presence of carotid plaque might be a good approach to stratify the risk of intracranial atherosclerosis progression in asymptomatic participants.Acknowledgements
We thank all the participants of the CAMERA (Cardio- and cerebrovascular Accident Monitoring, Epidemiology, and caRe quAlity system) study for their contribution.References
1. Shi Z, Li J, Zhao M, et al. Progression of Plaque Burden of Intracranial Atherosclerotic Plaque Predicts Recurrent Stroke/Transient Ischemic Attack: A Pilot Follow-Up Study Using Higher-Resolution MRI. J Magn Reson Imaging. 2021;54(2):560-570.
2. Xu Y, Li D, Yuan C, et al. Association of severity between carotid and intracranial artery atherosclerosis. Ann Clin Transl Neurol. 2018;5(7):843-849.
3. Mizukami H ST, Maki F, Shiraishi M, et al. Progression of intracranial major artery stenosis is associated with baseline carotid and intracranial atherosclerosis. J Atheroscler Thromb. 2015;22(2):183-190.Figures
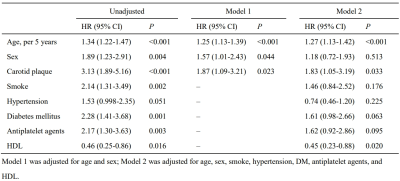
Table 1. Cox regression analyses for the
association between carotid plaque and the progression of intracranial atherosclerosis
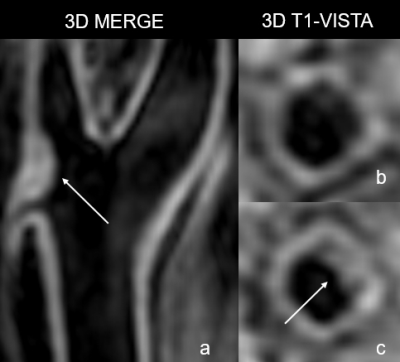
Figure
1. An example for a participant who had a carotid plaque at baseline and an
intracranial plaque at follow-up. A carotid plaque can be detected on 3D motion-sensitized
driven equilibrium prepared rapid gradient echo (3D MERGE) images at baseline (a, thin
arrow), and an intracranial plaque can be detected on 3D T1-weighted
volumetric isotropic turbo spin-echo acquisition (3D T1-VISTA) images at follow-up (c, thin
arrow), but without intracranial plaque at baseline (b).
DOI: https://doi.org/10.58530/2023/1346