1345
Visualization of the extracranial branches of the trigeminal nerve using iMSDE preparation 3D IR-TSE1Department of Radiology, First Affiliated Hospital of Fujian Medical University, Fuzhou, China, 2Department of Radiology, National Regional Medical Center, Binhai Campus of the First Affiliated Hospital, Fujian Medical University, Fuzhou, China, 3Key Laboratory of Radiation Biology of Fujian higher education institutions, First Affiliated Hospital, Fujian Medical University, Fuzhou, China, 4The School of Medical Imaging, Fujian Medical University, Fuzhou, China, 5Philips Healthcare, Shanghai, China, 6Department of Radiology, Fujian Key Laboratory of Precision Medicine for Cancer, First Affiliated Hospital of Fujian Medical University, Fuzhou, China
Synopsis
Keywords: Nerves, Nerves, magnetic resonance neurography; trigeminal nerve
Visualization of the anatomy of extracranial the trigeminal nerve (TGN) is crucial to detect nerve pathological alterations and differentiate pathologic causes. As a novel and safe nerve imaging technique in magnetic resonance neurography (MRN), the iMSDE pulse could result in uniform vascular signal suppression without additional contrast agents, which has been demonstrated to improve the visualization of peripheral nerves in several anatomical regions. Our results suggested that the iMSDE 3DIRTSE is a viable alternative to conventional 3DIRTSE and contrast-enhanced 3DIRTSE for MRN of the extracranial branches of TGN in clinical practice.Introduction
Visualization of the anatomy of extracranial TGN is crucial to detect nerve pathological alterations and differentiating pathologic causes 1-3. Due to high-field MRI devices and improved imaging techniques, magnetic resonance neurography (MRN) has become increasingly important in diagnosing neuropathies, which selectively enhances the visualization of nerves 4.As a novel and safe nerve imaging technique in MRN, the iMSDE pulse could result in uniform vascular signal suppression without additional contrast agents, which has been demonstrated to improve the visualization of peripheral nerves in several anatomical regions 5-7. However, there have been only limited studies in which the iMSDE 3DIRTSE sequence has been applied to delineate the peripheral branches of extracranial TGN 8.
Purpose
To compare the improved motion-sensitized driven equilibrium (iMSDE) 3DIRTSE (inverse recovery tuber spin echo) with conventional 3DIRTSE and the contrast-enhanced 3DIRTSE for magnetic resonance neurography (MRN) of the extracranial branches of the trigeminal nerve (TGN).Methods
In this prospective study, thirty-five subjects underwent the MRN of the TGN with conventional 3DIRTSE, iMSDE 3DIRTSE, and contrast-enhanced 3DIRTSE. MRI examinations were performed with a 3.0 T MRI unit (Philips Ingenia, Best, Netherlands). For qualitative analysis, the visibility of 6 major extracranial branches of trigeminal, venous suppression, muscle suppression, and identification ability of relationship between nerves and lesions was scored on a 5-point scale. For quantitative analysis, nerve signal-to-noise ratio (SNR), nerve-muscle contrast ratio (CRnm), nerve-venous CR (CRnv), nerve-muscle noise ratio (CNRnm) and nerve-venous CNR (CNRnv) were calculated and compared.Results
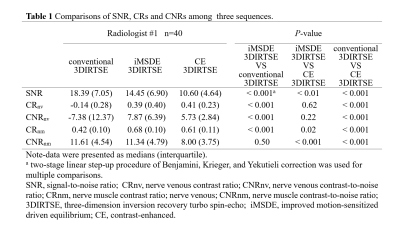
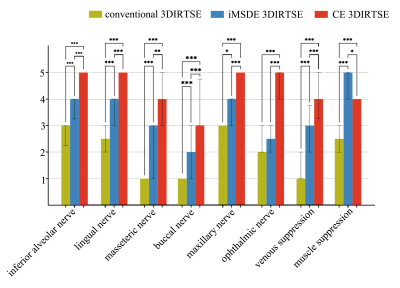
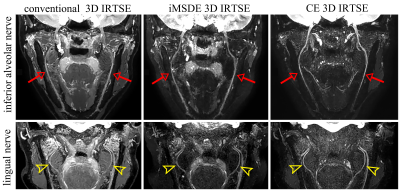
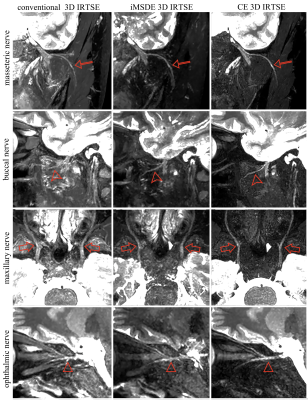
Images acquired with iMSDE 3DIRTSE had significantly higher CRnm, CRnv and CNRnv (all P<0.001) (table 1), better venous/muscle suppression and visualization of all TGN branches except ophthalmic nerve than conventional 3DIRTSE (all P<0.05) (Fig 1-3). The iMSDE 3DIRTSE had significantly higher SNR, CRnm and CNRnm of inferior alveolar nerve than did contrast-enhanced 3DIRTSE (all P<0.05). The CRnv and CNRnv were not statistically significant between iMSDE 3DIRTSE and contrast-enhanced 3DIRTSE (P=0.615, P=0.219, respectively). Compared with contrast-enhanced 3DIRTSE, iMSDE 3DIRTSE showed slightly lower scores for visualization of all TGN branches (all P<0.05), while having similar performance regarding acceptable diagnostic quality (scores≥3) of the inferior alveolar nerve, lingual nerve, masseteric nerve, and maxillary nerve (P>0.05). In identification ability of relationship between nerves and lesions, the iMSDE 3DIRTSE (5, 1.5) showed the highest scores compared with conventional 3DIRTSE (3, 2) and contrast-enhanced 3DIRTSE (2, 4) (all P<.05) (Fig 4).DISCUSSION
Our results demonstrated that iMSDE 3DIRTSE sequence provides improved venous suppression and nerve visualization than conventional 3DIRTSE in peripheral branches of TGN. And the visualization of the extracranial branches of TGN obtained by iMSDE 3DIRTSE is not inferior to contrast-enhanced 3DIRTSE. It suggested that the additional iMSDE pulse resulted in uniform venous and muscle suppression, enhancing the visualization of the nerve structures of the most TGN branches.Recently, the 3DIRTSE with iMSDE has been attempted to improve vessel signal suppression and visualization of nerves in brachial plexus based on the additional motion-sensitizing gradient field and T2 preparation pulse 5, 6, 9. However, the ophthalmic nerve remained challenging to visualize in iMSDE 3DIRTSE, despite iMSDE could enhance background tissue suppression. This can be explained by motion-sensitive nature of iMSDE preparation pulse, leading to unsatisfactory visualization of ophthalmic nerve caused by eye movement. In addition, the visualization score of the buccal nerve was relatively low in all three sequences. This discrepancy could be attributed to small nerve diameter and proximity to the pterygoid plexus.
Interestingly, our results showed that Gadolinium-Based Contrast Agents (GBCAs) could cause a signal reduction of contrast-enhanced lesions and damaged nerves, leading to a lower visualization effect for nerves-lesions relationship. The background tissue significantly decreased the signal based on the absorption of GBCAs and the nerve's signal is not affected because the blood-nerve barrier (BNB) blocked the contrast agent from the nerve tissue 10. It has been widely reported that contrast-enhanced 3DIRTSE had an excellent performance for the adequate assessment of the extracranial TGN branches anatomy. However, our preliminary findings demonstrated that contrast-enhanced 3DIRTSE had low contrast ratio between lesions and nerves due to significant signal reduction of the lesions, which is not conducive to the identification ability of the relationship between nerves and lesions. On the contrary, the qualitative analyses resulted in iMSDE 3DIRTSE having significantly higher scores in identification ability of nerve-lesion relationship than contrast-enhanced 3DIRTSE. The reason for this phenomenon may be that iMSDE preparation pulse did not cause significant decrease in signal of the lesions, yielding relative high contrast of nerves to lesions.
Conclusion
The iMSDE 3DIRTSE is a viable alternative to conventional 3DIRTSE and contrast-enhanced 3DIRTSE for visualization of the extracranial branches of TGN in clinical practice.Acknowledgements
No acknowledgement found.References
1. Cassetta M, Pranno N, Pompa V, Barchetti F, Pompa G. High resolution 3-T MR imaging in the evaluation of the trigeminal nerve course. Eur Rev Med Pharmacol Sci 2014; 18:257-264
2. Dessouky R, Xi Y, Zuniga J, Chhabra A. Role of MR Neurography for the Diagnosis of Peripheral Trigeminal Nerve Injuries in Patients with Prior Molar Tooth Extraction. AJNR Am J Neuroradiol 2018; 39:162-169
3. Cox B, Zuniga JR, Panchal N, Cheng J, Chhabra A. Magnetic resonance neurography in the management of peripheral trigeminal neuropathy: experience in a tertiary care centre. Eur Radiol 2016; 26:3392-3400
4. Bathla G, Hegde AN. The trigeminal nerve: an illustrated review of its imaging anatomy and pathology. Clin Radiol 2013; 68:203-213
5. Kasper JM, Wadhwa V, Scott KM, Rozen S, Xi Y, Chhabra A. SHINKEI--a novel 3D isotropic MR neurography technique: technical advantages over 3DIRTSE-based imaging. Eur Radiol 2015; 25:1672-1677
6. Klupp E, Cervantes B, Sollmann N, et al. Improved Brachial Plexus Visualization Using an Adiabatic iMSDE-Prepared STIR 3D TSE. Clin Neuroradiol 2019; 29:631-638
7. Srinivasan S, Hu P, Kissinger KV, et al. Free-breathing 3D whole-heart black-blood imaging with motion sensitized driven equilibrium. J Magn Reson Imaging 2012; 36:379-386
8. Van der Cruyssen F, Croonenborghs TM, Hermans R, Jacobs R, Casselman J. 3D Cranial Nerve Imaging, a Novel MR Neurography Technique Using Black-Blood STIR TSE with a Pseudo Steady-State Sweep and Motion-Sensitized Driven Equilibrium Pulse for the Visualization of the Extraforaminal Cranial Nerve Branches. AJNR Am J Neuroradiol 2021; 42:578-580
9. Yoneyama M, Takahara T, Kwee TC, Nakamura M, Tabuchi T. Rapid high resolution MR neurography with a diffusion-weighted pre-pulse. Magn Reson Med Sci 2013; 12:111-119
10. Wu W, Wu F, Liu D, et al. Visualization of the morphology and pathology of the peripheral branches of the cranial nerves using three-dimensional high-resolution high-contrast magnetic resonance neurography. Eur J Radiol 2020; 132:109137
Figures