1340
Automatic facial nerve tractography in patient with vestibular schwannoma1Center for Brain Imaging Science and Technology, College of Biomedical Engineering and Instrument Science, Zhejiang University, Hangzhou, China, 2Research Center for Healthcare Data Science, Zhejiang Lab, Hangzhou, China, 3Department of Neurosurgery, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China, 4University of Rochester, Rochester, NY, United States, 5School of physics, Zhejiang University, Hangzhou, China
Synopsis
Keywords: Nerves, Tractography & Fibre Modelling
Facial nerve tractography has recently been recognized as a valuable tool for predicting risk before vestibular schwannoma surgery to preserve function. Due to complexity of tissue structure, professional experience is usually required to manually adjust tracking parameters and place exclusion ROIs for optimal tractography. A pipeline for automatic facial nerve tractography will significantly lessen surgeons' workload. Here, we proposed a fiber growing method for adjusting the angle threshold adaptively and removed track outliers. Results show that the proposed method achieves good consistency with the manual method. The pipeline would have great potential for assisting clinic surgeries for vestibular schwannoma.
Introduction
Vestibular schwannoma (VS) develops on the vestibulocochlear nerve that passes from the inner ear to the brain. Surgery remains a challenge since it involves using sophisticated techniques in an area that is densely packed with nerves. In addition, the facial nerve may be compressed or stretched by VS, and it’s hardly to be seen clearly in routine MR images. Surgeons need to estimate orientation of the displaced facial nerve before surgery to preserve its function. Diffusion tractography can non-invasively illustrate specific nerve orientation before operation and help surgeons create an appropriate process for each patient1-3. Recent research has used Read-out Segmentation of Long Variable Echo-trains (RESOLVE) sequence to improve tractography outcomes, which can avoid distortions caused by traditional single-shot diffusion EPI sequences4. Although improvement in imaging sequences facilitates facial nerve tracking, manual interaction of parameter adjusting is usually required during tractography procedure. Especially in the presence of the tumor, facial nerve displaces far away from its known position due to compression. The operators need to set appropriate parameters and even visually select the facial nerve from messy streamlines to get the best track results.In order to simplify the procedure of fiber tracking and identification, this work proposes a growing method of facial nerve with an adaptive angle threshold and fiber cleaning strategy. The method can automate facial nerve tractography with good accuracy.
Methods
MRI images were obtained on a 3T Siemens Prisma scanner with a 64 channel head coil. Diffusion images were acquired using RESOLVE sequence with following settings: TR/TE=3000/48 ms, FOV=230x130 mm, voxel size=1.8 mm isotropic, segments=9, echo spacing=0.34 ms, b-value=800 mm2/s, 20 directions.High resolution anatomical images were acquired using T2-weighted 3D Turbo Spin Echo sequence with ZOOMit excitation with following settings: TR/TE=1000/128 ms, FOV=160x82x28 mm, voxel size=0.5 mm isotropic, turbo factor=80, echo spacing=7.36 ms, bandwidth=256 Hz/Px, average=3.5) for drawing the seed ROI.
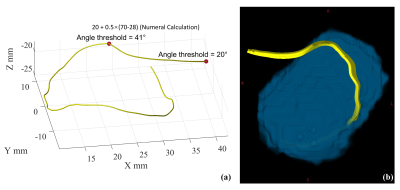
Post-processing on diffusion MRI data was performed using MRtrix3 for image denoising, eddy-current correction, motion distortion correction. For fiber-tracking, a seed ROI was manually placed in the internal acoustic meatus in the T2w image. Initial diffusion tensor tractography was then performed by MRtrix3 employing the deterministic tracking algorithm by using the fourth order Runge-Kutta method with the following parameters: FA cutoff = 0.12, maximum angle = 20°, number of streamlines = 50, and other with default setting. Fiber growiing started based on the initial results. For each streamline, the terminal point acted as a new seed point, and angle threshold (TA) was updated according to the following equation:
$$TA_{i}=TA_{i-1}+0.5*(FL_{exp}-FL_{i}),\ with\ TA<90°$$
where FLexp is expected fiber length (FL), depending on prior anatomical knowledge, FLi is current fiber length. Thus, the next tractography continues with the setting. Repeat this process and update the angle threshold until there meets the expected fiber length or angle threshold exceeds 90° to depict a reasonable fiber trajectory. The procedure is illustrated in Figure 1(a).
To clean streamlines into a compact facial nerve bundle, streamlines were removed that deviated from “core fiber”. “Core fiber” is calculated as the mean of each fiber x, y, z coordinates at each node5. We calculated Mahalanobis distance of each streamline and removed outliers. Finally, we segmented the tumor and showed position of facial nerve in relation to tumor in 3D view.
The pipeline have currently being tested on 38 patients in this study.
Results and Discussion
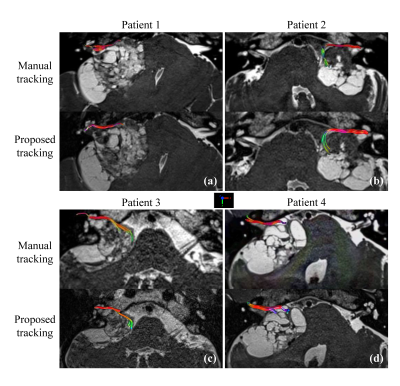
Facial nerve tractography in patient using pipeline above has been studied. Figure 1 shows process of fiber growing and the facial nerve bundle after cleaning in 3D view. In Figure 1(a), tractography began with a randomly selected seeding point from the drawn ROI, and stopped when reaching threshold limits. Then we adjusted angle threshold, according to equation above. Tracking continued from terminal point of the former segment under new constraints. We can repeat the growth process until desired fiber length was obtained.38 patients have been included in our study. For each patient, we tracked facial nerve of tumor side. Among them, 35 (92.1%) were successfully tracked, ie. 3 of facial nerves were not. Conditions that led to tractography failure were: large tumor (n=1), cystic tumor (n=1), and internal acoustic canal filling (n=1). 14 of them were compared with that used manual method. The latter was done by an operator that continuously adjusted parameters such as angle threshold to track longer fibers and placed multiple exclusion ROIs to discard spurious fibers. The results of manual method had been confirmed by surgeons. Figure 2 shows part of the two comparisons. It can be seen that our results are in high agreement with manual results. This means that it is possible to automate facial nerve tractography for a given seed ROI, which provides a convenient interface for surgeons.
Conclusion
The fiber growing method for adaptively adjusting the angle threshold and removing track outliers can significantly lessen the workload for surgeons, which achieved good consistency with the manual method. The pipeline would have great potential for assisting clinic surgeries for vestibular schwannoma.Acknowledgements
This work is supported by the National Natural Science Foundation of China (81871428).References
1. Ung N, Pelargos P E, Mozaffari K, et al. Accuracy and outcomes of diffusion tensor imaging tractography in resection for vestibular schwannoma for facial nerve preservation. Journal of the Neurological Sciences, 2021, 430: 120006.
2. Szmuda T, Słoniewski P, Ali S, et al. Reliability of diffusion tensor tractography of facial nerve in cerebello-pontine angle tumours. Neurologia i Neurochirurgia Polska, 2020, 54(1): 73-82.
3. Jacquesson T, Cotton F, Attyé A, et al. Probabilistic tractography to predict the position of cranial nerves displaced by skull base tumors: value for surgical strategy through a case series of 62 patients. Neurosurgery, 2019, 85(1): E125-E136.
4. Qiqi Tong, Ting Gong, Jing jin, et al. High Resolution Facial Nerve Tractography in Patient with Vestibular Schwannoma. ISMRM(2017), p3490.
5. Yeatman J D, Dougherty R F, Myall N J, et al. Tract profiles of white matter properties: automating fiber-tract quantification. PloS one, 2012, 7(11): e49790.
Figures