1336
Dynamic contrast-enhanced MRI-based interstitial fluid pressure model in evaluation of nasopharyngeal carcinoma1Department of Radiology, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangdong Key Laboratory of Nasopharyngeal Carcinoma Diagnosis and Therapy, Guangzhou, China, 2Shenzhen United Imaging Research Institute of Innovative Medical Equipment, Shenzhen, China, 3MR Collaboration, Central Research Institute, United Imaging Healthcare, Shanghai, China
Synopsis
Keywords: Head & Neck/ENT, Head & Neck/ENT
Nasopharyngeal carcinoma is cancer arising from the nasopharynx epithelium. The most widely researched etiological factor for nasopharyngeal carcinoma is the Epstein-Barr virus (EBV) infection. Elevated interstitial fluid pressure (IFP) is a significant biomarker for assessing head and neck malignant tumors. This study aimed to use the non-invasive dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI)-based IFP model to evaluate nasopharyngeal carcinoma and distinguish the differences between nasopharyngeal carcinoma patients with low and high EBV-infected levels. As a result, the non-invasive DCE-MRI-based IFP model could be used to evaluate nasopharyngeal carcinoma and differentiate patients with high- and low-level plasma EBV DNA.
Introduction
Nasopharyngeal carcinoma is cancer arising from the nasopharynx epithelium. Nasopharyngeal carcinoma has a distinct geographic distribution pattern compared to other cancer types, with the majority of new occurrences occurring in east and southeast Asia. The most widely researched etiological factor for nasopharyngeal carcinoma is the Epstein-Barr virus (EBV) infection. According to in-situ hybridization methods to EBV-encoded RNAs, the virus is only found in tumor cells and not in the healthy nasopharyngeal epithelium, indicating that EBV activation is crucial for the pathogenesis of nasopharyngeal carcinoma [1]. Elevated interstitial fluid pressure (IFP) is a significant biomarker for assessing head and neck malignant tumors [2]. A novel computational fluid modeling (CFM) based on dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) was reported to be used for IFP measurement of head and neck cancer [3]. This study aimed to use the non-invasive DCE-MRI-based IFP model to evaluate nasopharyngeal carcinoma and distinguish the differences between nasopharyngeal carcinoma patients with low and high EBV-infected levels.Methods
A total of 66 patients (45 men, 21 women; mean age, 47 years; age range, 20–77 years) with histologically confirmed nasopharyngeal carcinoma between April 2020 and April 2022 were recruited in this research. The inclusion and exclusion criteria were as follows. Inclusion criteria: 1) recently diagnosed as non-keratinizing undifferentiated nasopharyngeal carcinoma; 2) pre-treatment MRI examinations were performed; 3) the pre-treatment plasma EBV deoxyribonucleic acid (DNA) was recorded. Exclusion criteria: 1) history of head or neck radiotherapy or previous chemotherapy; 2) degraded image quality or obvious motion artifacts; 3) cystic lesions or massive necrosis within the tumor.MRI examination was performed on a 3.0T scanner (uMR 790, United Imaging Healthcare, Shanghai, China). DCE-MRI was performed in 70 phases per examination using axial dynamic three-dimensional gradient recalled echo sequence with 0.2 mL/kg, 0.5 mmol/mL gadolinium (Multihance) administration (repetition time (TR) = 3.64 ms; echo time (TE) = 1.3 ms; flip angle (FA) = 10°; field-of-view (FOV) = 255 × 256 mm2; matrix = 258 × 288; slice thickness = 2.5 mm; number of slices = 32).
IFP was estimated by applying CFM, considering both osmotic and hydrostatic pressure and capillary hydraulic conductivity. Pharmacokinetic modeling of DCE-MRI provided physiologically relevant markers of perfusion and permeability [4]. The continuity partial differential equation to describe the physiological processes (Starling law and Darcy law) was combined and solved with the finite element method [3]. Finally, the IFP map depicted the heterogeneity within the tumor, stemming from the incorporation of Ktrans to inform fluid influx rate variability from the spatial contrast agent extravasation. Regions of interest (ROIs) were manually contoured within the edge of the tumor, avoiding areas of necrosis and hemorrhage. Pearson’s correlation was applied to evaluate the relationship between the plasma EBV DNA and the mean IFP value. The two-sample t-test was performed to compare the mean IFP value between the low-level group and the high-level group. P-value less than 0.05 was considered statistically significant.
Results
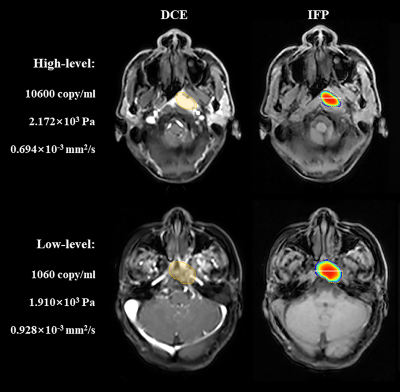
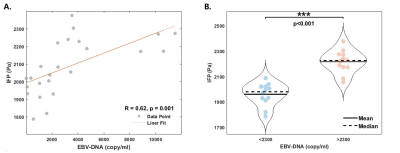
Thirty-two patients (48%) had plasma EBV DNA ≥ 2300 copies/mL, and 34 patients (52%) had plasma EBV DNA <2300 copies/mL. Representative DCE-MRI images and corresponding IFP maps of a patient with high EBV-infected level (Male, 48 years old) and a patient with low EBV-infected level (Female, 51 years old) were shown in Fig. 1. As shown in Fig.2, the mean IFP value was significantly positively correlated with the plasma EBV DNA (Pearson’s rho = 0.62, P = 0.001). The mean IFP value could differentiate patients with high-level (≥2300 copies/mL) plasma EBV DNA and patients with low-level (<2300 copies/mL) plasma EBV DNA (AUC = 0.911, sensitivity = 97%, specificity = 74%).Discussion
Elucidating the impact of the EBV-infected microenvironment will be helpful to promote the individualized treatment of nasopharyngeal carcinoma patients and improve the prognosis. In the current study, significant correlations between the pre-treatment plasma EBV DNA and mean IFP value was found. The factors that caused IFP abnormalities in tumors involved vascular leakage, lymphatic abnormalities, interstitial fibrosis, and contractive interstitial space [5]. High IFP in the internal environment of malignant tumors was the consequence of severe microvascular and interstitial abnormalities [6]. Our results inferred that the EBV-infected microenvironment with high IFP might facilitate EBV DNA cloning and EBV-infected cell reproduction.Conclusion
In conclusion, the non-invasive DCE-MRI-based IFP model could be used to evaluate nasopharyngeal carcinoma and may contribute to individualized treatment and prognosis of nasopharyngeal carcinoma.Acknowledgements
No acknowledgement found.References
1. Chua, Melvin LK, et al. "Nasopharyngeal carcinoma." The Lancet 387.10022 (2016): 1012-1024.
2. Gutmann, Ralph, et al. "Interstitial hypertension in head and neck tumors in patients: correlation with tumor size." Cancer research 52.7 (1992): 1993-1995.
3. LoCastro, Eve, et al. "Computational modeling of interstitial fluid pressure and velocity in head and neck cancer based on dynamic contrast-enhanced magnetic resonance imaging: feasibility analysis." Tomography 6.2 (2020): 129-138.
4. Shukla-Dave, Amita, et al. "Dynamic contrast-enhanced magnetic resonance imaging as a predictor of outcome in head-and-neck squamous cell carcinoma patients with nodal metastases." International Journal of Radiation Oncology* Biology* Physics 82.5 (2012): 1837-1844.
5. Heldin, Carl-Henrik, et al. "High interstitial fluid pressure—an obstacle in cancer therapy." Nature Reviews Cancer 4.10 (2004): 806-813.
6. Jain, Rakesh K. "Delivery of molecular medicine to solid tumors: lessons from in vivo imaging of gene expression and function." Journal of controlled release 74.1-3 (2001): 7-25.
Figures