1335
Radiomics model based on MRI for early prediction of radiation encephalopathy in nasopharyngeal carcinoma
Lixuan Huang1, Zongxiang Yang1, Hao Ren2, Yao Hu1, Cheng Tang1, Huiting Zhang3, and Liling Long1
1The First Affliated Hospital of Guangxi Medical University, Nanning, China, 2Guangxi Medical University Kaiyuan Langdong Hospital, Nanning, China, 3MR Scientific Marketing, Siemens Healthineers Ltd, Wuhan, China
1The First Affliated Hospital of Guangxi Medical University, Nanning, China, 2Guangxi Medical University Kaiyuan Langdong Hospital, Nanning, China, 3MR Scientific Marketing, Siemens Healthineers Ltd, Wuhan, China
Synopsis
Keywords: Head & Neck/ENT, Radiomics
This study aimed to develop radiomic models based on MRI to investigate the changes of temporal lobe heterogeneity in nasopharyngeal carcinoma (NPC) patients with radiation encephalopathy (REP) during the latent period, and to predict the temporal lobe REP early. Results showed that The AUC of radiomics-clinics combined model was higher than radiomics model and clinics model, with better accuracy. Our study suggested that the radiomics-clinics combined model may be an effective method for the noninvasive prediction of REP in NPC patients after radiotherapy.Introduction/Purpose
Most nasopharyngeal carcinoma (NPC) are highly sensitive to radiotherapy, and radiotherapy has become the first choice for the treatment of NPC1. Therefore, radiation encephalopathy (REP) in the temporal lobe has become the most likely neurological complication after radiotherapy for nasopharyngeal carcinoma, with a prevalence ranging from 4 % to 18%2-3, and its impact on the quality of life of patients has far exceeded that brought about by the tumor itself. The American Cancer Society Center emphasized that in order to maximize the quality of life of cancer patients after comprehensive treatment, the prevention and treatment of complications in cancer treatment strategies should be the top priority of future research4. Therefore, REP has received increasing attention, and the prediction of latent REP early in the incubation period is of decisive significance in the final prognosis5. This study aimed to establish radiomic models based on MRI to investigate the changes of temporal lobe heterogeneity in NPC patients with REP during the latent period, and to predict the temporal lobe radiation encephalopathy early.Methods
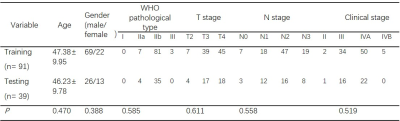
130 NPC patients receiving radiotherapy, 80 REP-positive and 50 REP-negative patients, were retrospectively enrolled between January 2010 and August 2022. Age, sex, pathologic type, TN staging were collected as clinical factors. MR examinations of all patients with before treatment and the end of treatment were collected. MR data included T1WI, T1WI_CE and T2WI. ITK-SNAP software was used to manually sketch and segment the volume of interest (VOI) of medial temporal lobe on the MR T1WI, T1WI_CE and T2WI by two experienced doctors. The imaging features were analyzed and extracted by using FeAture Explorer (V 0.3.6) on Python (3.7.6)6. We used computer-generated random numbers to assign 70% of the patients to the training cohort (n= 91) and the others to the testing cohort (n= 39). Before build the model, recursive feature elimination (RFE) for selecting features and linear discriminant analysis (LDA) or LASSO constrain as the classifier were adopted. Cross validation with 5-fold on the training data set was used to determine the hyper-parameter, which was set according to the model performance on the validation data set. The discrimination result of the model was obtained by bootstrap. The area under the ROC curve (AUC), accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were performed to evaluate the model performance in both the training and testing cohorts.Results
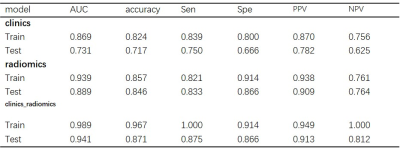
Characteristics differences between Training and Testing NPC group are shown in Table 1. The AUC of radiomics-clinics combined model and radiomics model reached to 0.989 (95% CI:0.976—1.000) and 0.939[95% CI: 0.895—0.982] for training cohort, and the corresponding AUC in testing cohort were 0.941 (95% CI: 0.875—1.000) and 0.889 (95% CI: 0.782—0.994) for combined and radiomics model, respectively. All of them were higher than clinics model (AUC=0.869 and 0.731 for training and Test cohort, respectively). The accuracy of combined model for REP-positive in NPC was higher than clinics model (0.967 vs. 0.824). It was also suggested improvement in combined model compared to radiomics model (0.967 vs. 0.857). More details are shown in Table 2 and Figure 1-3.Discussion and Conclusion
This study was to determine if there is a difference between radiomics features based on MR from temporal lobe heterogeneity for NPC patients with REP-positive and REP-negative at the end of radiotherapy. The most important is to predict the temporal lobe radiation encephalopathy early. The radiomics-clinics combined model and radiomics model showed good performances in training cohort and testing cohort. Their accuracy was better than clinics model. In conclusion, our study suggested that the radiomics-clinics combined model may be an effective method for the noninvasive prediction of REP in NPC patients after radiotherapy.Acknowledgements
We sincerely thank the participants in this study.References
[1]. Langendijk JA, Leemans CR, Buter J, et al. The additional value of chemotherapy to radiotherapy in locally advanced nasopharyngeal carcinoma: a meta-analysis of the published literature. J Clin Oncol. 2004;22: 4604–12. [2]. Su SF, Huang Y, Xiao WW, et al. Clinical and dosimetric characteristics of temporal lobe injury following intensity modulated radiotherapy of nasopharyngeal carcinoma. Radiother Oncol. 2012; 104:312–6. [3] Chen WS, Li JJ, Zhang JH, et al. Magnetic resonance spectroscopic imaging of brain injury after nasopharyngeal cancer radiation in early delayed reaction. Genet Mol Res. 2014; 13:6848–6854. [4] Tang Y, Luo D, Rong X, Shi X, Peng Y, et al. Psychological dis-orders, cognitive dysfunction and quality of life in nasopharyngeal carcinoma patients with radiation-induced brain injury. PLoS One. 2012; 7: e36529. [5] Zhang B, Lian ZY, Zhong LM, et al. Machine-learning based MRI radiomics models for early detection of radiation-induced brain injury in nasopharyngeal carcinoma BMC Cancer. 2020; 20: 502. [6] Song, Y., et al., FeAture Explorer (FAE): A tool for developing and comparing radiomics models. PLoS One, 2020. 15(8): e0237587.Figures
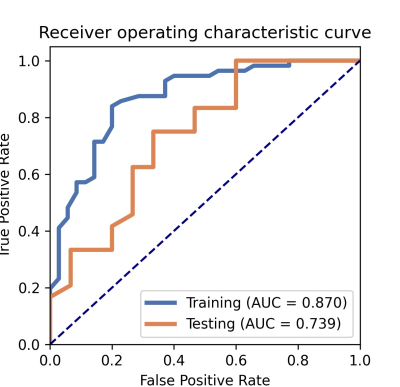
Figure 1. Receiver operating characteristic curves (ROC) analyses of the clinics model.
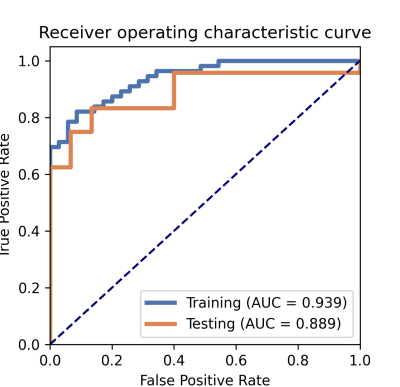
Figure 2. Receiver operating characteristic curves (ROC) analyses of the radiomics model.
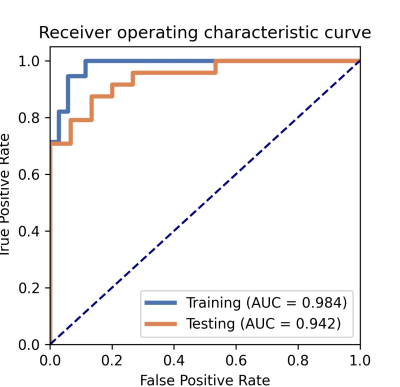
Figure 3. Receiver operating characteristic curves (ROC) analyses of the radiomics-clinics
combined model.
Table
1. Characteristics differences between Training and Testing NPC were determined
using the T-test (age) or chi-square test (Classification variables, *: P <
0.05.).
Table
2. Performance of clinics, radiomics and combine models in NPC patients with REP-positive.
DOI: https://doi.org/10.58530/2023/1335