1327
Factors Affecting Outcomes in Nonischemic Dilated Cardiomyopathy: Development and Validation of a CMR-Based Nomogram1Fuwai Hospital and National Center for Cardiovascular Diseases, Beijing, China, 2Union Hospital of Fujian Medical University, Fujian, China
Synopsis
Keywords: Cardiomyopathy, Cardiomyopathy
Risk evaluation for patients with NIDCM remains an important public health challenging, and new techniques and strategies are expected to be used to prevent cardiac death. This study was designed to develop and validate a novel nomogram score to predict outcomes in patients with NIDCM over a long follow-up time period.Purpose
Effective and specific risk evaluation for patients with nonischemic dilated cardiomyopathy (NIDCM) remains challenging. Thus, this study aimed to develop and validate a novel nomogram score to predict outcomes in NIDCM patients.Methods
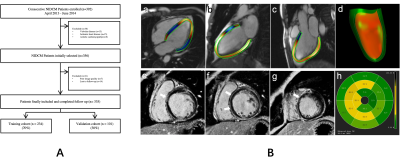
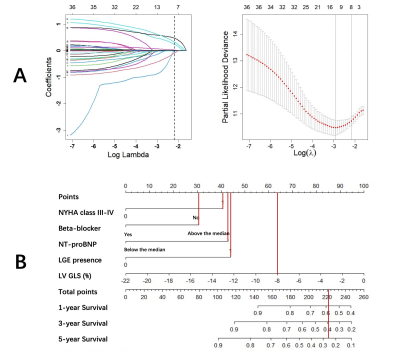
A total of 335 consecutive NIDCM patients who underwent cardiac magnetic resonance (CMR) imaging were retrospectively enrolled. Comprehensive clinical evaluation and imaging investigation were obtained, including measurements of late gadolinium enhancement(LGE) and feature tracking(FT) strain. All patients were followed up for a composite endpoint of major adverse cardiac events(MACE) including all-cause mortality and heart transplantation. These patients were randomly divided into training and validation cohort(7:3). LASSO regression analysis were utilized to identify prognostic factors. A nomogram based on the selected predictive variables was built to predict MACE.Results
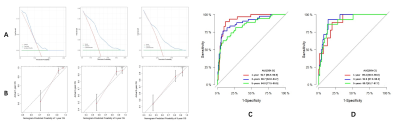
MACE occurred in 93 out of 234 patients in the training cohort, and in 41 out of 101 patients in the validation cohort. Six variables including NYHA class, NT-proBNP, Beta-blocker medication, LGE presence, and LV global longitudinal strain(GLS) were found to be significantly associated with MACE and were used for constructing the nomogram. The nomogram achieved good discrimination with C-indexes of 0.80 and 0.82 in the training and validation cohorts, respectively. The calibration curve for 1-, 3-, and 5-year survival also showed high coherence between the predicted and actual probability of MACE. Decision curve analysis identified the model was clinically useful in predicting MACE.Conclusion
This study presents a predictive model that incorporates traditional clinical factors and CMR parameters, which can be conveniently used to facilitate the risk stratification in NIDCM.Acknowledgements
This study was made possible by the wonderful work of colleagues in department of Magnetic Resonance Imaging, Fuwai hospital, Beijing, China.References
[1] Weintraub RG, Semsarian C, Macdonald P. Dilated cardiomyopathy[J]. Lancet, 2017,390(10092):400-414. DOI:10.1016/S0140-6736(16)31713-5.
[2] Japp AG, Gulati A, Cook SA, et al. The diagnosis and evaluation of dilated cardiomyopathy[J]. J Am Coll Cardiol,2016,67(25):2996-3010. DOI: 10.1016/j.jacc.2016.03.590.
[3] Halliday BP, Cleland JGF, Goldberger JJ, et al. Personalizing risk stratification for sudden death in dilated cardiomyopathy: Thepast, present, and future[J]. Circulation, 2017,136(2):215-231. DOI: 10.1161/CIRCULATIONAHA.116.027134.
[4] Smiseth OA, Torp H, Opdahl A, et al. Myocardial strain imaging: How useful is it in clinical decision making?[J]. Eur Heart J,2016,37(15):1196-1207. DOI: 10.1093/eurheartj/ehv529.
[5] Romano S, Judd RM, Kim RJ, et al. Feature-tracking global longitudinal strain predicts death in a multicenter population ofpatients with ischemic and nonischemic dilated cardiomyopathy incremental to ejection fraction and late gadoliniumenhancement[J]. JACC Cardiovasc Imaging, 2018,11(10):1419-1429. DOI: 10.1016/j.jcmg.2017.10.024.
[6] Chimura M, Onishi T, Tsukishiro Y, et al. Longitudinal strain combined with delayed-enhancement magnetic resonanceimproves risk stratification in patients with dilated cardiomyopathy[J]. Heart, 2017,103(9):679-686. DOI: 10.1136/heartjnl-2016-309746.
[7] Cleland JGF, Halliday BP, Prasad SK. Selecting Patients With Nonischemic Dilated Cardiomyopathy for ICDs: Myocardial Function, Fibrosis, and What's Attached? J Am Coll Cardiol. 2017 Sep 5;70(10):1228-1231. DOI: 10.1016/j.jacc.2017.07.748.
[8] Deng Y, Zhang N, Hua W, et al. Nomogram predicting death and heart transplantation before appropriate ICD shock in dilated cardiomyopathy. ESC Heart Fail. 2022 Apr;9(2):1269-1278. DOI: 10.1002/ehf2.
[9] Patel AR, Kramer CM. Role of Cardiac Magnetic Resonance in the Diagnosis and Prognosis of Nonischemic Cardiomyopathy. JACC Cardiovasc Imaging. 2017 Oct;10(10 Pt A):1180-1193. DOI: 10.1016/j.jcmg.2017.08.005.
Figures