1324
Lung water estimation using cardiac magnetic resonance imaging for predicting adverse cardiovascular outcomes in patients with heart failure1Dept of cardiovascular radiology and Endovascular interventions, All India institute of medical sciences, Delhi, India, 2Dept of cardiovascular radiology and Endovascular interventions, All India institute of medical sciences, Delhi, Delhi, India, 3Dept of Cardiovascular radiology and Endovascular interventions, All India institute of medical sciences, Delhi, Delhi, India
Synopsis
Keywords: Heart, Lung, Heart failure
The present study sought to determine whether CMR-derived lung water density (LWD) measurement in pulmonary congestion has prognostic relevance in predicting adverse cardiovascular outcomes in patients with heart failure. The primary endpoint was all-cause mortality or HF-related hospitalization within 6 months from CMR.
It concluded -
1. The mean lung water density was significantly higher in heart failure patients compared to healthy controls.
2. Patients with “wet lungs” i.e., lung water density >18.1%, had higher incidence of adverse cardiovascular outcomes compared to patients with “dry lungs”.
3. Lung water density was an independent predictor of adverse cardiovascular outcomes
Objectives
Pulmonary congestion is a central feature of heart failure (HF), seen in acute decompensated state as well as in chronic stable disease. Cardiac magnetic resonance imaging (CMR) is a non-invasive, promising tool for assessing lung water content.The present study sought to determine whether simplified CMR-derived lung water density (LWD) measurement has prognostic relevance in predicting adverse cardiovascular outcomes in patients with HF and left ventricular ejection fraction (LVEF)<50%.
Introduction
Heart failure (HF) is characterized by structural and functional abnormalities of the myocardium that result in impaired ventricular filling or ejection of blood. (1)Hemodynamic parameters include preload, cardiac output and afterload. Increase in preload is represented by increased pulmonary capillary wedge pressure (PCWP) which is an independent predictor of poor prognosis in patients with HF. (2) Increased PCWP leads to engorgement of the pulmonary and bronchial vasculature leading to transudation of fluid into the interstitial and alveolar space with increase in the extravascular lung water (EVLW). (3) Thus, measurement of lung water can predict deterioration and decompensation at an early stage and guide institution of appropriate treatment.
Lung water quantification on CMR has previously been validated against gravimetric methods. (4,5)
Materials and Methods
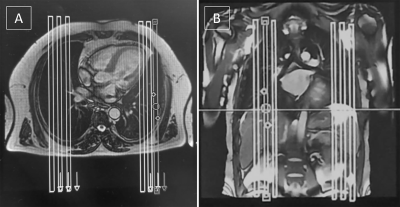
Eighty consecutive patients referred for CMR with HF and LVEF<50% along with 22 healthy age- and sex-matched controls were prospectively recruited.LWD was measured using half-Fourier single shot turbo spin-echo (HASTE; Half Fourier Single-shot Turbo Spin-Echo) pulse sequence. The imaging parameters included matrix size of 128 x 74 with a 360 x 270 mm field of view, 8 mm slice thickness, 6/8th partial Fourier, 3.2 ms echo spacing, 67 ms echo time and 120° pulse flip angle. Six sagittal slices covering the right and left lung were acquired in end-expiratory breath-hold to minimise variation in lung signal due to inflation (Figure 1). (14) Scan time for lung water estimation was ~37 seconds.
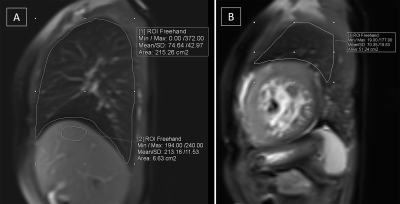
LWD was the lung-to-liver signal intensity ratio multiplied by 70% (estimated hepatic water density). The primary endpoint was composite of all-cause mortality or HF-related hospitalisation within 6 months from CMR.
Results
The mean LWD was significantly higher in HF patients compared to healthy controls (19.78 ± 6.1 vs. 13.6 ± 2.3; p<0.001). The mean LWD was significantly different among patients with NYHA class I/II and NYHA class III/IV (17.88 ± 4.8 vs. 21.77 ± 1.08; p=0.004). At 6 months, the primary endpoint was reached in 12 (15%) patients. Patients with “wet lungs” (LWD>18.1%) had higher incidence of adverse cardiovascular outcomes compared to patients with “dry lungs”. LWD was an independent predictor of adverse cardiovascular outcomes in multivariable analysis. At the optimal cut-off of LWD>23.38%, the sensitivity and specificity were 91.67% and 91.18%, respectively to predict adverse cardiovascular outcomes.Conclusion
LWD on CMR is independently associated with increased risk of mortality and HF-related hospitalization in HF patients with LVEF<50%.Acknowledgements
No acknowledgement found.References
1. Inamdar AA, Inamdar AC (2016) Heart Failure: Diagnosis, Management and Utilization. J Clin Med 5(7):E62.
2. Aalders M, Kok W (2019) Comparison of Hemodynamic Factors Predicting Prognosis in Heart Failure: A Systematic Review. J Clin Med 8(10):E1757.
3. Chase SC, Taylor BJ, Cross TJ, Coffman KE, Olson LJ, Johnson BD (2017) Influence of Thoracic Fluid Compartments on Pulmonary Congestion in Chronic Heart Failure. J Card Fail 23(9):690–6.
4. Mayo JR, MacKay AL, Whittall KP, Baile EM, Paré PD (1995) Measurement of lung water content and pleural pressure gradient with magnetic resonance imaging. J Thorac Imaging 10(1):73–81.
5. Hayes CE, Case TA, Ailion DC, et al (1982) Lung water quantitation by nuclear magnetic resonance imaging. Science 216(4552):1313–5.
Figures