1318
Sex differences between total cerebral blood flow and age-related changes in the brain using 4D flow MRI1Medical Physics, University of Wisconsin- Madison, Madison, WI, United States, 2Radiology, University of Wisconsin- Madison, Madison, WI, United States, 3Wisconsin Alzheimer's Institute, University of Wisconsin- Madison, Madison, WI, United States, 4Wisconsin Alzheimer's Disease Research Center, University of Wisconsin- Madison, Madison, WI, United States, 5Geriatric Research Education and Clinical Center, William S. Middleton Memorial Veterans Hospital, Madison, WI, United States
Synopsis
Keywords: Flow, Aging
Vascular disease is strongly associated with Alzheimer’s disease. Therefore, it is important to establish normative cerebrovascular changes in aging populations. In this study, we assess sex-specific, age-related changes in total cerebral blood flow (tCBF) and total parenchymal volume in 754 cognitively healthy, older adults. We further investigate whether the same changes are observed in flow normalized by total parenchymal volume. We found (1) significant decrease in tCBF and total parenchymal volume with age in both sexes, (2) no correlation between age and normalized flow in male subjects, and (3) significant decrease in normalized flow with age in female subjects.Introduction
“Normal” vascular aging is known to occur with decreased perfusion, meanwhile, brain volumes and associated decreased metabolic demand are also occurring concurrently. This is particularly relevant to cerebrovascular and neurologic health as cardiovascular disease risk factors are associated with dementia risk, including not only vascular dementia1 but also Alzheimer’s disease (AD) and related dementias (ADRD). It is essential to study the relationship of “normal” vascular aging and cerebrovascular disease (CVD) to neurodegeneration as the aging population and the projected impact of ADRD increases. Non-invasive, reproducible, quantitative vascular measures are needed to both study “normal” vascular aging and CVD. To begin to accomplish these larger goals, the primary aims of this study are (1) to investigate associations of total cerebral blood flow (tCBF) and total parenchymal volume with age and sex and (2) determine if these associations are impacted by normalizing flow by total parenchymal volume.Methods
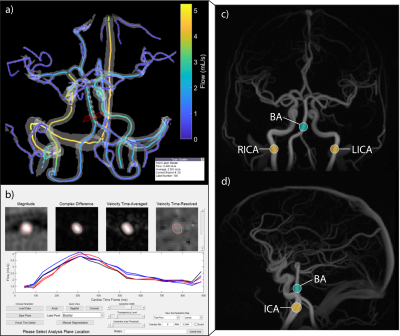
Cohort consisted of 754 cognitively healthy subjects (503F/251M; mean age=64y; age range=[45-93y]) from the Wisconsin Alzheimer’s Disease Research Center (Figure 1). 4D flow MRI data were acquired on three separate 3T clinical systems (GE Healthcare, Waukesha, WI): Discovery MR750 with a 32-channel head coil (N=561) or 8-channel head coil (N=46), Signa MR/PET with an 8-channel coil (N=8), or Signa Premier using a 48-channel coil (N=139). A non-contrast, radially-undersampled 4D flow sequence (PCVIPR2,3) acquisition was used with the following parameters: TR/TE=6.9-8.3/2.5-3.0ms; flip=8°; projections=11,000; isotropic resolution=0.69mm; image volume=22x22x10cm3; VENC=80cm/s; velocity encode scheme=4-point (N=320) or 5-point (N=434); scan time=5.6min or 7.1min, depending on encoding scheme. The data was reconstructed into 20 cardiac frames using retrospective peripheral pulse oximeter gating and temporal radial view sharing4. An interactive, semi-automated 4D flow processing tool (Figure 2), developed in Matlab2020b (Mathworks, Natick, MA), was used to measure mean volumetric flow rates in cervical internal carotid arteries (ICA) and basilar artery (BA). Flow rates from ICAs and BA were summed giving tCBF in mL/min. White matter (WM) and grey matter (GM) volumes were automatically segmented from T1-weighted MPRAGE and T2-weighted images using SPM125. Total parenchymal volume was computed as the sum of WM and GM volumes, measured in mL. tCBF was normalized by total parenchymal volume (normalized tCBF), expressed in mL of blood per 100 mL of brain parenchyma per min (mL/100 mL/min). Two sample t-tests were performed to compare (1) age, (2) tCBF, (3) total parenchymal volumes, and (4) normalized tCBF between male and female subjects. Simple linear regression models, in two groups (male and female subjects), were used to assess correlations between age and each outcome variable (tCBF, total parenchymal volume, and normalized tCBF).Results
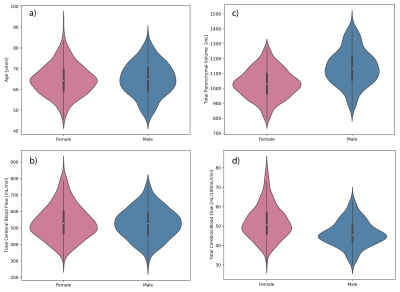
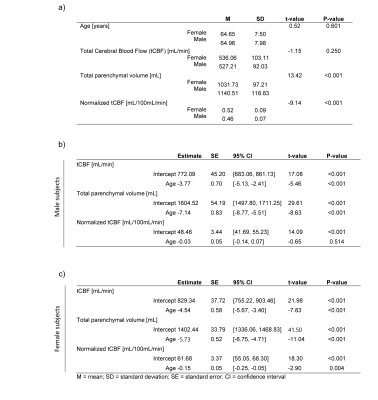
All 754 subjects were successfully processed, with tCBF and total parenchymal volume measurements obtained. There was no significant difference in age between male and female subjects. Linear regression models showed an inverse correlation between age and tCBF (βFemale = -4.54; βMale = -3.77; p < 0.001; Figure 3a). There was no significant correlation between sex and tCBF (p = 0.250). There was an inverse correlation between age and total parenchymal volumes (βFemale = -5.73; βMale= -7.14; p < 0.001: Figure 3b). There was a significant difference in total parenchymal volumes between male subjects (M = 1140.51 mL, SD = 118.83 mL) and female subjects (M = 1031.73 mL, SD = 97.21 mL) (p < 0.001). The correlation between age and tCBF was no longer observed when tCBF was normalized (βMale = -0.03; p = 0.514) in male subjects, while age was still strongly correlated with normalized tCBF in female subjects (βFemale = -0.15; p = 0.004) (Figure 3c).Discussion
We found a significant association between tCBF and age, corresponding to an annual flow decrease of 3.77 mL/min in male, and 4.54 mL/min in female subjects. We observed no correlation between sex and tCBF, suggesting that there is no significant difference in tCBF between female and male subjects. There was a strong correlation between age and decrease in total parenchymal volumes, corresponding to an annual decrease of 7.14 mL in male, and 5.73 mL in female subjects. As expected, there was a significant difference in total parenchymal volumes between male and female subjects, indicating higher average brain size in male subjects. All these results confirm findings from other studies6–10. Es et al. reported no significant changes in normalized flow with age7. Our study differs in cohort size, CVD status, and subjects’ age range, and unlike Es et al., we investigated sex specific correlations of normalized flow with age. Male subjects exhibited no significant change in normalized flow with age, suggesting that tCBF is likely driven by atrophy. However, significant annual decrease of normalized flow was observed in female subjects, suggesting other mechanisms at play such as post-menopausal vascular changes11. Further investigation on the relationship between tCBF changes and menopause onset age is needed. This is the largest study that showed sex-specific differences in correlation between age and normalized tCBF.Conclusion
4D flow MRI was successfully used to measure total cerebral blood flow (tCBF) in a large cohort of cognitively normal older subjects. We show significant decrease of tCBF and total parenchymal volume with age and demonstrate that the decrease of normalized tCBF is only present in female subjects.Acknowledgements
Research reported in this abstract was supported by the National Institutes of Health (NIH) under award numbers F31AG071183, KL2TR002374, UL1TR002373, R01AG075788, RF1AG027161, P30AG062715, R21AG077337, TL1TR002375, and the Alzheimer’s Association under award number AARFD-20-678095. The content is solely the responsibility of the authors and does not necessarily represent the official views of these institutions. We would like to thank GE Healthcare for their continued technical assistance and product support. We also gratefully acknowledge the researchers and staff at the Wisconsin Institutes for Medical Research, Wisconsin Alzheimer’s Disease Research Center, and Waisman Brain Imaging Core for assistance in recruitment, data collection, and data analysis. Lastly, the authors extend their most sincere thanks to all participants involved in this study.References
1. Samieri, C. et al. Association of Cardiovascular Health Level in Older Age With Cognitive Decline and Incident Dementia. JAMA 320, 657–664 (2018).
2. Gu, T. et al. PC VIPR: a high-speed 3D phase-contrast method for flow quantification and high-resolution angiography. AJNR Am J Neuroradiol 26, 743–9 (2005).
3. Johnson, K. M. et al. Improved 3D phase contrast MRI with off-resonance corrected dual echo VIPR. Magn Reson Med 60, 1329–1336 (2008).
4. Liu, J. et al. Generation and visualization of four-dimensional MR angiography data using an undersampled 3-D projection trajectory. IEEE Trans Med Imaging 25, 148–57 (2006).
5. Schmidt, P. et al. An automated tool for detection of FLAIR-hyperintense white-matter lesions in Multiple Sclerosis. Neuroimage 59, 3774–83 (2012).
6. Buijs, P. C. et al. Effect of age on cerebral blood flow: measurement with ungated two-dimensional phase-contrast MR angiography in 250 adults. Radiology 209, 667–74 (1998).
7. van Es, A. C. G. M. et al. Associations between total cerebral blood flow and age related changes of the brain. PLoS One 5, e9825 (2010).
8. Scheel, P., Ruge, C., Petruch, U. R. & Schöning, M. Color Duplex Measurement of Cerebral Blood Flow Volume in Healthy Adults. Stroke 31, 147–150 (2000).
9. Amin-Hanjani, S., Du, X., Pandey, D. K., Thulborn, K. R. & Charbel, F. T. Effect of age and vascular anatomy on blood flow in major cerebral vessels. J Cereb Blood Flow Metab 35, 312–8 (2015).
10. Fotenos, A. F., Mintun, M. A., Snyder, A. Z., Morris, J. C. & Buckner, R. L. Brain volume decline in aging: evidence for a relation between socioeconomic status, preclinical Alzheimer disease, and reserve. Arch Neurol 65, 113–20 (2008).
11. Wong, R. H. X., Evans, H. M. & Howe, P. R. C. Poor cerebrovascular function is an early marker of cognitive decline in healthy postmenopausal women. Alzheimers Dement (N Y) 2, 162–168 (2016).
Figures