1243
4D flow MRI for investigation of fetal cardiovascular hemodynamics in healthy development and ductal dependent lesions1Radiology, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States, 2Radiology, Children's Hospital Colorado, Aurora, CO, United States, 3Pediatric Cardiology, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States
Synopsis
Keywords: Fetal, Velocity & Flow
Fetal cardiovascular MRI has the potential to aid in the diagnosis and evaluation of congenital heart disease. Here, a fast, Doppler ultrasound- gated, 4D flow MRI acquisition with online reconstruction was achieved in twelve healthy fetuses and six patients with suspected congenital cardiovascular defects. Analysis of the 4D flow data revealed expected flow distributions across vascular territories in the healthy cohort. Using 4D flow MRI, we were also able to evaluate the presence and impact of ductal dependent lesions in patients with suspected congenital heart disease, finding confirmation of presence/absence of pathology on post-natal imaging.Introduction
The fetal cardiovascular system has several distinctive features that work together to deliver oxygenated blood from the placenta to the fetus. One such feature, the ductus arteriosus (DA) connects the main pulmonary artery (MPA) to the proximal descending aorta (DAo), directing pulmonary blood away from the fluid filled lungs towards the systemic circulation. In coarctation of the aorta (CoA), a ductal dependent lesion characterized by narrowing of the aortic isthmus region, postnatal closure of the DA on day 2-3 of life reveals the impact of the aortic narrowing, leading to obstruction of blood flow to abdominal organs and extremities and requiring urgent intervention. CoA remains difficult to diagnose on fetal echocardiography due to the proximity of the ductal and aortic arches.MRI can provide a comprehensive assessment of vessel blood flow. Prior studies evaluating fetal blood flow used multiple, carefully placed individual 2D phase contrast (PC) planes1 or employed an iteration of the slice-to-volume approach, acquiring multi-planar, multi-slice 2D PC-MRI reconstructed in 3D2. These prior implementations required careful plane placement (often necessitating rescans to obtain the appropriate vessel), long acquisition times, and offline reconstruction. Here, the purposes are to (1) demonstrate the utility of a fast, Doppler ultrasound-gated 4D flow MRI acquisition and online reconstruction to visualize and quantify fetal circulatory hemodynamics in healthy development, and (2) evaluate the clinical value of fetal 4D flow MRI in suspected ductal dependent lesions.
Methods
With IRB approval, 12 healthy pregnant volunteers (gestational age, GA=35±2 weeks) and six patients with suspected congenital cardiovascular abnormalities from fetal echocardiography (GA=36±1 weeks) were prospectively recruited and scanned at 1.5T (n=2) or 3T (n=16) (Philips). Fetal cardiac gating was obtained with a MR-compatible Doppler ultrasound device (Northh Medical)3,4. Localizers covering the entire fetus were acquired and segmented to determine fetal body mass5. 4D flow data encompassing the fetal heart and major vessels were acquired with a fixed acquired resolution=2.5mm isotropic, FOV=[200-360×200-360×40-87.5]mm3, temporal resolution=41-50ms, acquired cardiac phases=10, VENC=150cm/s, TR=2.85-3.29ms, TE=1.67-2.07ms, flip angle=6°, SENSE=2×1.5 (phase×slice), and scan time=132-217s.Using EnSight (Ansys), flow was quantified in three adjacent planes separated by ~1mm in six vascular territories (Fig1). The mean across measurement planes for each territory was normalized by fetal mass to obtain flow in mL/min/kg, or by combined ventricular output (CVO=MPA+ascending aorta (AAo) flow) to compute relative segmental flow. To evaluate reliability, the within-subject coefficient of variation (WS-CV) was computed across adjacent measurement planes, and repeatability of quantified flow was evaluated from two repeated acquisitions in two volunteers.
Patient comparison: Flow rates were measured in clinically relevant vessels for each patient and compared to the reference standards established by the healthy volunteer cohort. When available, features were compared to postnatal CT or echocardiography exams.
Results
Healthy volunteers: The mean±SD fetal mass was 2393±325g and fetal heart rate was 135±9bpm. Fig2 shows a representative fetal 4D flow path-line visualization and Fig3 summarizes flow in the major vessels. Mean CVO was 238±47 mL/min/kg. As expected in these healthy fetuses, flow decreases from AAo to isthmus due to branching head vessels, and branch pulmonary artery blood flow (PBF=MPA-DA) was low due to high pulmonary vascular resistance. DAo flow was increased post ductal and aortic arch convergence. Repeatability analysis showed that in all segments, WS-CV<18%, and hemodynamic parameters quantified from repeated 4D flow acquisitions had good agreement (Fig4).Ductal dependent lesions: 4D flow MRI was successfully acquired in all patients.
Suspected pulmonary atresia (n=1): 4D flow demonstrated absence of antegrade pulmonary arterial flow, reverse flow in the DA and symmetric distribution of flow into right and left pulmonary arteries, consistent with pulmonary atresia. Postnatal CT confirmed these findings (Fig5-Top).
Suspected hypoplastic aortic arch or CoA (n=5): In two cases, increased ductal flow and reverse flow in the aortic arch was observed on 4D flow, indicative of CoA. Postnatal CT confirmed these findings in one case (Fig5-Bottom) and the second is pending delivery. One case, suspected of long segment coarctation, instead revealed a focal coarctation at the aortic isthmus (case pending delivery). In the remaining two, normal distribution of flow through the aortic arch and ductus arteriosus was found, ruling out ductal dependance. A normal arch was observed on the postnatal echocardiography in one ‘ruled out’ case, and the other is pending delivery.
Discussion
4D flow MRI was successfully used to evaluate the fetal circulation in healthy development and ductal dependent lesions. Importantly, these data were acquired in ~3 min and reconstructed online (vs 14-30 min for prior approaches and requiring offline reconstruction1,2). In the presence of substantial fetal motion, 4D flow data can be corrupted, however with this method, it leads to the loss of gating signal and suspension of data collection as well.In healthy fetuses, relative flow distributions across major vessels agree within 10% of the 2D PC reference ranges previously reported1. Absolute flow by 4D flow MRI may be underestimated compared to prior studies1,2 due to partial volume artifacts, however we contend that the clinically important ability to evaluate fetal blood flow directionality and circulatory distributions is retained.
In conclusion, fetal 4D flow is feasible in third trimester patients and has potential to better inform diagnosis in suspected ductal dependent lesions.
Acknowledgements
Supported by NIH/NCATS Colorado CTSA Grant Number KL2 TR002534 and seed funding from the Colorado Fetal Care Center.References
1. Prsa M, Sun L, van Amerom J, Yoo SJ, Grosse-Wortmann L, Jaeggi E, Macgowan C, Seed M. Reference ranges of blood flow in the major vessels of the normal human fetal circulation at term by phase-contrast magnetic resonance imaging. Circ Cardiovasc Imaging. 2014 Jul;7(4):663-670.
2. Roberts TA, van Amerom JFP, Uus A, Lloyd DFA, van Poppel MPM, Price AN, Tournier JD, Mohanadass CA, Jackson LH, Malik SJ, Pushparajah K, Rutherford MA, Razavi R, Deprez M, Hajnal JV. Fetal whole heart blood flow imaging using 4D cine MRI. Nat Commun. 2020 Oct 5;11(1):4992. Doi: 10.1038/s41467-020-18790-1. Erratum in: Nat Commun. 2020 Dec 14;11(1):6413.
3. Kording F, Yamamura J, de Sousa MT, Ruprecht C, Hedström E, Aletras AH, Ellen Grant P, Powell AJ, Fehrs K, Adam G, Kooijman H, Schoennagel BP. Dynamic fetal cardiovascular magnetic resonance imaging using Doppler ultrasound gating. J Cardiovasc Magn Reson. 2018; 20:17.
4. Kording F, Schoennagel BP, de Sousa MT, Fehrs K, Adam G, Yamamura J, Ruprecht C. Evaluation of a Portable Doppler Ultrasound Gating Device for Fetal Cardiac MR Imaging: Initial Results at 1.5T and 3T. Magn eason Med Sci. 2018;17:308-317.
5. Baker PN, Johnson IR, Gowland PA, Hykin J, Harvey PR, Freeman A, Adams V, Worthington BS, Mansfield P. Fetal weight estimation by echo-planar magnetic resonance imaging. Lancet. 1994; 343(8898):644–645.
Figures
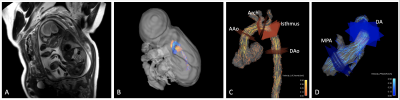
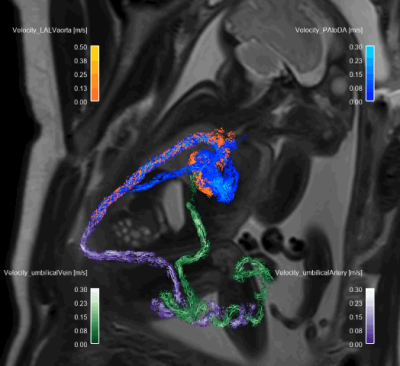
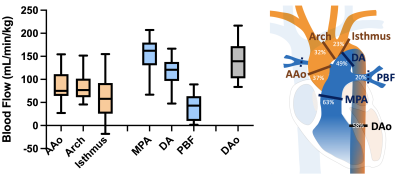
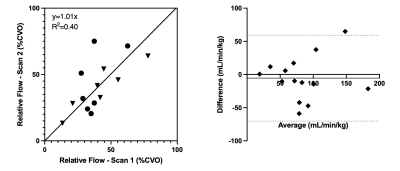
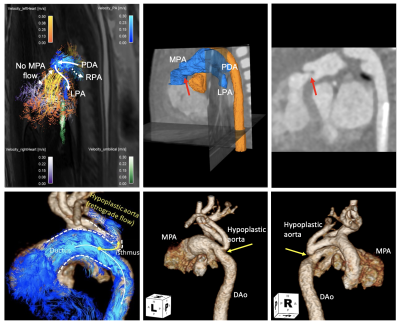
Figure 5. (Top) Left: 4D flow MRI in patient with pulmonary atresia (GA=37 weeks) showed absence of antegrade pulmonary arterial flow, instead relying on retrograde flow through the patent DA to supply the left and right pulmonary arteries. Center & Right: Post-natal CT exam confirmed pulmonary atresia (red arrow).
(Bottom) Left: 4D flow MRI in patient with hypoplastic arch and CoA (GA=34 weeks) overlaid on post-natal CT. Retrograde flow is seen in the hypoplastic arch and into the supra-aortic vessels. Center & Right: Two views of post-natal CT confirm MR findings.