1200
MR neurography Aids in Detection of Longitudinal Brachial Plexus Nerve Root Alterations in Patients With Amyotrophic Lateral Sclerosis1Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China, 2Philips Healthcare, Shanghai, China, 3UT Southwestern Medical Center, Dallas, TX, United States
Synopsis
Keywords: Nerves, Nerves
We assessed proximal-distal longitudinal signal and size alterations of brachial plexus nerve roots in amyotrophic lateral sclerosis (ALS) patients using 3D nerve-sheath signal increased with inked rest-tissue rapid acquisition of relaxation enhancement imaging (3D SHINKEI) . The conclusion confirmed proximal-distal longitudinal diameters and SNR values decreased significantly for brachial plexus nerve roots in ALS patients with larger differences in slopes compared to the HC. Thus, the size and signal alterations of brachial plexus nerve roots using 3D SHINKEI can be used to supplement clinical diagnosis for ALS patients.Introduction
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disorder characterized by upper and lower motor neuron loss of the human nervous system, leading to progressive weakness of the bulbar, limb, thoracic and abdominal muscles [1]. However, a lack of sensitivity of these criteria and the heterogeneous clinical presentation as well as varying speed of progression makes clinical diagnosis of ALS challenging [2; 3]. Neuropathology studies show lesions of peripheral nerves in ALS, especially in brachial plexus, including axonal degeneration, neuroinflammation, and wallerian degeneration of fibers [4]. Therefore, detecting imaging abnormality of brachial plexus may serve as a diagnostic marker in ALS. Magnetic resonance neurography (MRN) has been widely used in the diagnosis of peripheral neuropathy [5; 6], providing structural information to complement the functional information of neurophysiologic tests. Three-dimensional nerve-sheath signal increased with inked rest-tissue rapid acquisition of relaxation imaging (3D SHINKEI) is a novel MRN sequence that includes a combination of two prepulses and 3D turbo spin-echo sequence with T2-weighting. It enables vascular signal suppression and superior 3D visualization of detailed anatomy of the brachial plexus in high spatial resolution [7; 8]. However, ALS patients have not been assessed quantitatively on imaging or using 3D SHINKEI. The aim of this study was to assess the proximal-distal longitudinal signal and size alterations of the brachial plexus roots using nerve-selective sequence, 3D SHINKEI and to investigate whether the imaging features are helpful in differentiating ALS patients from HCs.Methods
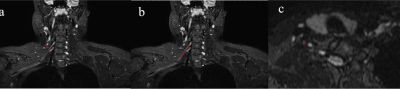
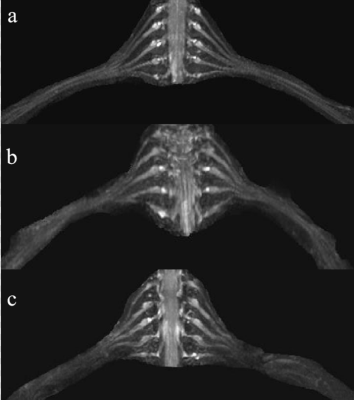
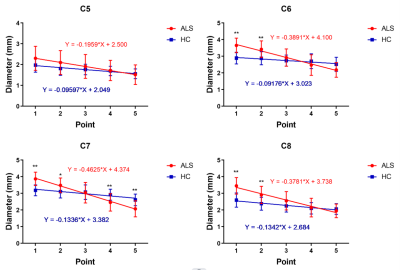
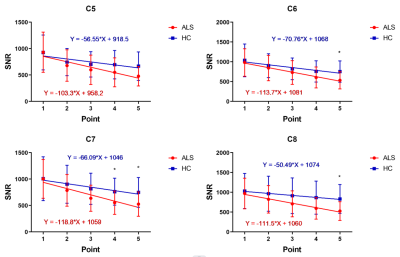
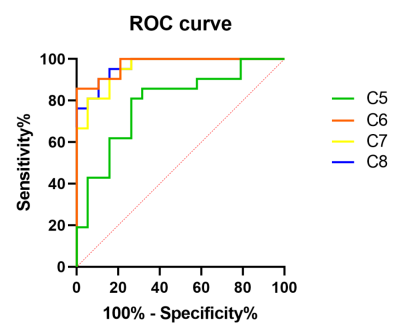
21 ALS patients and 19 healthy controls (HC) were evaluated by using 3D SHINKEI. The diameters and signal-to-noise ratio (SNR) values of C5-C8 roots were measured at five points from proximal to distal sites( Figure1). Student’s t test was performed to compare the differences at each point between the two groups. Linear regression was performed for each nerve root, and the differences of linear regression slopes between two groups were analyzed. Receiver operating characteristic (ROC) analysis was performed for the diameter ratio of the distal to the proximal points.Results
Interobserver agreement was excellent. The diameters and SNR values of C5-C8 roots from proximal to distal showed significant changes (p<0.05) except the SNR value of C5 root of HC. The decrease in slopes were larger in ALS patients than HC in C5-C8 nerve roots (p<0.05) except the SNR values of C5 and C7 nerve roots (Figure 2,3,4). The ROC analysis confirmed that the diameter ratio could differentiate ALS patients from HC with high accuracy (Figure 5).Discussion
In this study, the results of 3D SHINKEI imaging reveal that the diameters and SNR values of C5-C8 roots from proximal to distal decreased significantly and in ALS more than HCs. These results indicate the root alterations are different between proximal and distal points. The ROC results further revealed the diameter ratio of distal point to proximal point could distinguish ALS from healthy controls with high sensitivity and specificity, suggesting that it is a potential surrogate imaging marker for ALS. Potential etiologies for these findings could include neuroinflammation, endothelial dysfunction, and nerve edema [9] occurring during the ALS course. The proximal nerve enlargement might be related to this neuroinflammation and consequent nerve edema and swelling. Interestingly, the results further indicated that the diameters and SNR values of nerve roots at the distal points were decreased compared to controls, which could be a result of reduced myelinated fibers and chronic axonal degeneration [4]. Given that ALS is a motor neuronopathy, progressive motor axonal degeneration and nerve fiber loss is considered to be a major cause of signs and symptoms in ALS [10; 11].Therefore, the differences from proximal to distal may be related with different disease stages. In this study, one ALS patient imaged 72.3 months after the onset of symptoms demonstrated entire brachial plexus atrophy including the proximal roots, reflecting chronicity of disease process and the late stage of the ALS pathogenetic cascade. This patient was excluded from our study as the markedly atrophic nerve roots were unclear on 3D SHINKEI. Further prospective study with a larger number of patients is needed to ascertain whether this change observed in 3D SHINKEI images is systematically associated with disease course and severity.There have been controversies in the literature regarding the diameters of nerve roots of ALS patients. Most ultrasound studies suggest that the roots were thinner in ALS patients [12], while increased diameters have been found on the MRI studies. This study systematically evaluated the nerve roots at different segments from proximal to distal parts, and found that the signal and size alterations were different, which may account for the controversies above. 3D SHINKEI allowed excellent nerve selective imaging and depiction of the above-described lesions. This also contributed to excellent inter-reader reliability in both signal and size measurements despite the small size of the nerves.Conclusion
Proximal-distal longitudinal diameters and SNR values decreased significantly for brachial plexus nerve roots in ALS patients with larger differences in slopes compared to the HC. Thus, the size and signal alterations of brachial plexus nerve roots using 3D SHINKEI can be used to supplement clinical diagnosis for ALS patients.Acknowledgements
The scientific guarantor of this publication is Guangbin Wang. The authors declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work was supported by Natural Science Foundation of Shandong Province (Nos.ZR2019PH08). No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. No study subject or cohort was previously reported.References
1. Turner MR, Swash M (2015) The expanding syndrome of amyotrophic lateral sclerosis: a clinical and molecular odyssey. J Neurol Neurosurg Psychiatry 86:667-6732
2. Diagnosis ETFo, Management of Amyotrophic Lateral S, Andersen PM et al (2012) EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)--revised report of an EFNS task force. Eur J Neurol 19:360-3753
3. Campanari ML, Bourefis AR, Kabashi E (2019) Diagnostic Challenge and Neuromuscular Junction Contribution to ALS Pathogenesis. Front Neurol 10:684
4. Sobue G, Matsuoka Y, Mukai E, Takayanagi T, Sobue I (1981) Pathology of myelinated fibers in cervical and lumbar ventral spinal roots in amyotrophic lateral sclerosis. J Neurol Sci 50:413-4215
5. Kronlage M, Baumer P, Pitarokoili K et al (2017) Large coverage MR neurography in CIDP: diagnostic accuracy and electrophysiological correlation. J Neurol 264:1434-14436
6. Fortanier E, Ogier AC, Delmont E et al (2020) Quantitative assessment of sciatic nerve changes in Charcot-Marie-Tooth type 1A patients using magnetic resonance neurography. Eur J Neurol 27:1382-13897
7. Kasper JM, Wadhwa V, Scott KM, Rozen S, Xi Y, Chhabra A (2015) SHINKEI--a novel 3D isotropic MR neurography technique: technical advantages over 3DIRTSE-based imaging. Eur Radiol 25:1672-16778 8. Yoneyama M, Takahara T, Kwee TC, Nakamura M, Tabuchi T (2013) Rapid high resolution MR neurography with a diffusion-weighted pre-pulse. Magn Reson Med Sci 12:111-1199
9. Stoll G, Muller HW (1999) Nerve injury, axonal degeneration and neural regeneration: basic insights. Brain Pathol 9:313-32510
10. Riva N, Chaabane L, Peviani M et al (2014) Defining peripheral nervous system dysfunction in the SOD-1G93A transgenic rat model of amyotrophic lateral sclerosis. J Neuropathol Exp Neurol 73:658-67011
11. Devigili G, Uceyler N, Beck M et al (2011) Vasculitis-like neuropathy in amyotrophic lateral sclerosis unresponsive to treatment. Acta Neuropathol 122:343-35212
12. Mori A, Nodera H, Takamatsu N et al (2016) Sonographic evaluation of cervical nerve roots in ALS and its clinical subtypes. J Med Invest 63:54-57
Figures