1198
Analysis of cerebral perfusion changes after microvascular decompression in patients with hemifacial spasm1China-Japan Friendship Hospital, Beijing, China
Synopsis
Keywords: Nerves, Brain
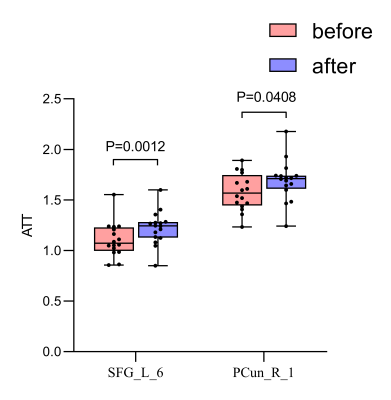
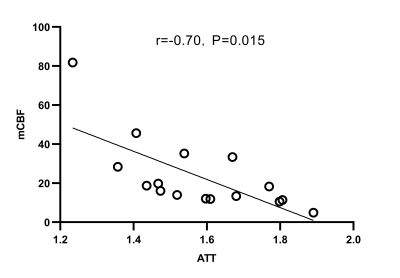
We used the eASL technique to explore the mCBF, ATT and CBV alterations after MVD in patients with HFS. And found that the ATT values in the left superior frontal gyrus region 6 and the right precuneus region 1 were significantly increased in the L-HFS group after surgery compared with the preoperative ones. Furthermore, preoperative ATT values in the right precuneus 1 region were negatively correlated with mCBF values in the L-HFS group. It is suggested that these brain regions may play different roles in the underlying pathological mechanisms of HFS.Background or Purpose
Hemifacial spasm (HFS) is an involuntary contraction syndrome of facial muscles innervated by ipsilateral facial nerves, which can gradually affect facial expressive muscles and platysma muscles[1]. The currently accepted etiology of HFS is the long-term neurovascular compression at the root exit zone of the facial nerve, which leads to abnormal excitation of the facial nerve nucleus or abnormal transmission of nerve fiber telecommunications signals[2]. The microvascular decompression (MVD) is the first choice of surgery for HFS[3]. The purpose of this study was to explore the mean cerebral blood flow (mCBF), arterial passage time (ATT) and cerebral blood volume (CBV) alterations after MVD in patients with HFS using enhanced arterial spin labeling (eASL) technique. We hypothesized that some alterations in these cerebral perfusion parameters would occur in patients with HFS. Since long-term chronic facial spasm may produce psychological problems such as anxiety or depression[4], so we evaluated some relevant psychological scales. In addition, we explored the correlation between altered cerebral perfusion parameters and clinical information.Methods
26 patients, 11 males and 15 females, aged 27-69 (53.31±10.07) years, enrolled from May 2022 to August 2022 in the Department of Neurosurgery, China-Japan Friendship Hospital. All patients received MVD, and the eASL data and Cohen's spasticity intensity grading, Self-Assessment Scale (SAS), Self-Rating Scale of Depression (SDS), and Self-Rating Sleep Status Scale (SRSS) data were collected before and 5-7 days after surgery, respectively. The patients were divided into the left HFS (L-HFS) group (16 patients) and the right HFS (R-HFS) group (10 patients) according to the location of the facial spasm. CereFlow software was used for data post-processing to obtain cerebral blood perfusion parameters for each brain region: mCBF, ATT and CBV. Data were visualized using the MATLAB-based Brainnetome Atlas software package. Paired-samples t-test was used to compare the parameters of mCBF, ATT and CBV in each group of HFS patients before and after surgery. Pearson correlation analysis was used to evaluate the correlation between mCBF, ATT and CBV in parameter-altered brain regions between them and clinical scale scores.Results
The ATT values in the left superior frontal gyrus region 6 and the right precuneus region 1 were significantly increased in the L-HFS group after surgery compared with the preoperative ones [(1.22±0.17)s compared with (1.11±0.17)s and (1.69±0.20)s compared with (1.58±0.18)s; all FDR-corrected P<0.05] (Figure 1); the differences of all parameters in the remaining brain regions were not statistically significant (all FDR-corrected). The differences in cerebral perfusion parameters in all brain regions were not statistically significant in the R-HFS group (all FDR-corrected P>0.05). Preoperative ATT values in the right precuneus 1 region were negatively correlated with mCBF values in the L-HFS group (r=-0.70, P=0.015, FDR-corrected) (Figure 2);. There was no correlation between cerebral perfusion parameters and clinical scale scores in the remaining differential brain regions (all FDR-corrected P>0.05).Conclusions
In primary HFS, the ATT was altered in several brain regions after MVD compared to preoperative and these alterations were correlated with the mCBF. It is suggested that these brain regions may play different roles in the underlying pathological mechanisms of HFS.Acknowledgements
The authors thank Dr. Lizhi Xie from GE Healthcare for help in solving MR technical problems.References
[1] Gao W, Yang D, Zhang Z, et al. Altered Cortical-Striatal Network in Patients With Hemifacial Spasm. Front Hum Neurosci. 2021;15:770107. Published 2021 Oct 22. doi:10.3389/fnhum.2021.770107
[2] Green KE, Rastall D, Eggenberger E. Treatment of Blepharospasm/Hemifacial Spasm. Curr Treat Options Neurol. 2017;19(11):41. Published 2017 Sep 30. doi:10.1007/s11940-017-0475-0
[3] Li J, Lyu L, Chen C, Yin S, Jiang S, Zhou P. The outcome of microvascular decompression for hemifacial spasm: a systematic review and meta-analysis. Neurosurg Rev. 2022;45(3):2201-2210. doi:10.1007/s10143-022-01739-x
[4] Bao F, Wang Y, Liu J, et al. Structural changes in the CNS of patients with hemifacial spasm. Neuroscience. 2015;289:56-62. doi:10.1016/j.neuroscience.2014.12.070