1194
MRI Assessment of the Therapeutic Effect of Combined Electroacupuncture and Stem Cells in Acute Peripheral Nerve injury1Department of radiology, Shenzhen Traditional Chinese Medicine Hospital, Shenzhen, China, 2Department of pathology, Shenzhen Traditional Chinese Medicine Hospital, Shenzhen, China, 3MR Collaboration, SIEMENS Healthineers Ltd., Beijing, China, 4Department of Nuclear Medicine, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, China
Synopsis
Keywords: Nerves, Nervous system, Electroacupuncture, Mesenchymal stem cells
We aimed to verify the efficacy of bone mesenchymal stem cells (BMSCs) combined with electroacupuncture (EA) in the treatment of peripheral nerve injury (PNI) using pathology and MRI. In a rat model of sciatic nerve crush damage, we found that BMSCs and EA combined therapy improved axon and myelin regeneration synergistically and significantly decreased post-injury nerve edema, improved axon guiding factor, and expedited motor function recovery. This suggests that a combination of BMSCs and EA can provide both topological and biomolecular guidance to promote axonal extension, myelin regeneration, and functional recovery after PNI.Introduction
Peripheral nerve injury (PNI) is a prevalent clinical condition characterized by sensory and motor deficits. Bone mesenchymal stem cell (BMSC) transplantation has emerged as a novel and promising candidate strategy for the treatment of PNI but remains limited. Electroacupuncture (EA) has been widely utilized for PNI rehabilitation due to its relative simplicity, affordability, and safety in comparison to other conventional therapies1. Recent studies on cerebral ischemic disease revealed that grafted BMSCs and EA treatment combined significantly enhanced the functional recovery of motor and cognitive deficits compared to BMSCs or EA treatment alone. This provides a valuable method for treating peripheral nerve injuries, but further validation is needed. This study was proposed to monitor axonal extension, myelin regeneration, and functional recovery after PNI using pathology and MRI to verify the efficacy of BMSCs combined with EA in the treatment of PNI.Materials and Methods
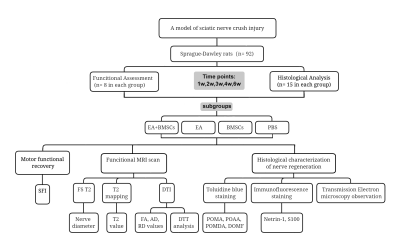
Ninety-two healthy adult male Sprague-Dawley rats sustained an acute crush injury to the left sciatic nerve, and were randomly divided into the EA+BMSCs group (A), EA group (B), BMSCs group (C), or PBS group (control) (D). Rats in groups A and B received EA by stimulating Huantiao (GB30) and Zusanli (ST36)2, 3. Rats in groups A and C received subepidermal microinjections of 5×105 BMSCs suspended in phosphate-buffered saline (PBS) with a final volume of 3.0 μL, whereas animals in group D got the same volume of PBS as controls. At each time point of 0, 1, 2, 3, 4, and 6 weeks, T2 values and diffusion tensor imaging (DTI) derived from multiparametric magnetic resonance imaging (MRI), histological assessments, and immunohistochemistry were used to monitor nerve regeneration. Walking track analysis was used to assess nerve functional recovery. Repeated-measures one-way analysis of variance was used to evaluate the significance of T2, DTI, and SFI values among the four groups. One-way analysis of variance was used for comparing the histological characteristics. Bonferroni test was used for multiple pairwise comparisons at each time point.Results
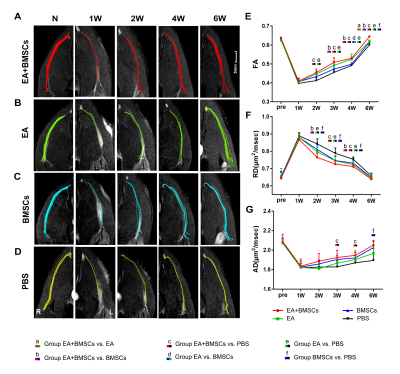
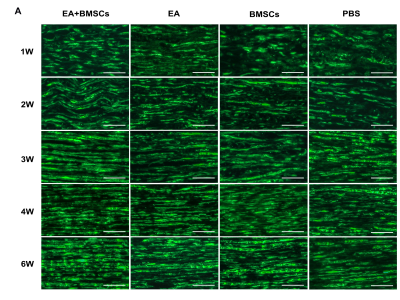
Figure 1 shows the experimental timeline and flowchart of the experiment. Figure 2, and Figure 3 show the MRI and histological characterizations at each time point in EA+BMSCs, EA, BMSCs, and PBS groups. In terms of fractional anisotropy (FA), the EA+BMSCs and EA groups had faster recovery than PBS (control) at all time points after surgery, and the EA+BMSCs group recovered better than the BMSCs group at three weeks (P≤0.008) (Figure 2). FA values were higher in the EA group than in the BMSCs group at four weeks (P≤0.008). In terms of radial diffusivity (RD), the EA+BMSCs group recovered better than the BMSCs group at two and four weeks (P≤0.008). Immunofluorescence staining for axon guidance molecule Netrin-1 revealed that it was significantly higher in the EA+BMSCs subgroup and EA subgroup than it was in the control (PBS) subgroup at 1-3 weeks (P<0.001) (Figure 4). Immunofluorescence staining for S100 showed the continuity of nerve fibers recovered more quickly in the EA+BMSCs subgroup than in the BMSCs subgroup (Figure 5).Discussion
In a rat model of sciatic nerve crush damage, we found that BMSCs and EA combined therapy improved axon and myelin regeneration synergistically. Meanwhile, the combined therapy significantly decreased post-injury nerve edema, improved axon guiding factor, and expedited motor function recovery. According to our data, however, even untreated injury-model rats (PBS group) displayed nerve self-healing potential, and the BMSCs alone treatment group did not demonstrate a substantial functional recovery advantage. Several factors may contribute to the inadequate efficacy of stem cell therapy in PNI. A small percentage of the transplanted BMSCs survived for up to eight weeks. What’s more, BMSCs could elicit a humoral and cellular immune response in vivo and promote inflammation when the immune system is under-activated4, 5. This may explain the slower rate of edema reduction and debris removal in the stem cell-alone group. In our investigation, the combination of BMSCs with EA yielded the most effective therapeutic outcomes, including optimal myelin and axonal regeneration and recovery of nerve function. It suggests that EA not only increases the regeneration of myelin and axons by itself, but also enhances the efficacy of stem cells by enhancing their survival, migration, paracrine function, and neural differentiation. In terms of several histological parameters of nerve fiber regeneration and sciatic nerve function index, the EA-only group demonstrated superior or equal efficacy compared to the stem cell-only group. This demonstrates that electroacupuncture has distinct benefits in the treatment of peripheral neuropathy, is non-invasive and inexpensive, and should be promoted as a therapy approach.Cobclusion
In conclusion, our research revealed that a combination of BMSCs and EA can provide both topological and biomolecular guidance to promote axonal extension, myelin regeneration, and functional recovery after PNI. EA not only promotes nerve repair on its own but also enhanced the beneficial effects of stem cell treatment.Acknowledgements
No acknowledgement found.References
1. Wu Q, Chen J, Yue J, et al. Electroacupuncture improves neuronal plasticity through the A2AR/cAMP/PKA signaling pathway in SNL rats. Neurochem Int, 2021,145:104983.
2. Perreault T, Fernández-de-Las-Peñas C, Cummings M, et al. Needling Interventions for Sciatica: Choosing Methods Based on Neuropathic Pain Mechanisms-A Scoping Review. J Clin Med, 2021,10(10).
3. Yu FT, Liu CZ, Ni GX, et al. Acupuncture for chronic sciatica: protocol for a multicenter randomised controlled trial. BMJ Open, 2022,12(5):e54566.
4. Ankrum JA, Ong JF, Karp JM. Mesenchymal stem cells: immune evasive, not immune privileged. Nat Biotechnol, 2014,32(3):252-260.
5. Jiang W, Xu J. Immune modulation by mesenchymal stem cells. Cell Prolif, 2020,53(1):e12712.
Figures