1150
The Effect of Respiratory and Cardiac Motion States on B0 Shimming at 3T
Yuheng Huang1,2, Xingmin Guan1, Xinheng Zhang1,2, Liqi(Richard) Tang 1, Ghazal Yoosefian1, Xiaoming Bi3, Fei Han3, HsuLei Lee4, Hui Han4, Anthony Christodoulou4, Debiao Li4, Rohan Dharmakumar1, and Hsin-Jung Yang4
1krannert cardiovascular research center, Indiana University school of medicine, Indianapolis, IN, United States, 2Bioengineering, UCLA, LA, CA, United States, 3Siemens Healthineers, Malvern, PA, United States, 4Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States
1krannert cardiovascular research center, Indiana University school of medicine, Indianapolis, IN, United States, 2Bioengineering, UCLA, LA, CA, United States, 3Siemens Healthineers, Malvern, PA, United States, 4Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States
Synopsis
Keywords: Artifacts, High-Field MRI, Motion-resolved field map, cardiac shimming
B0 inhomogeneity imposes imaging artifacts on CMR images and compromises the reliability of popular B0-sensitive sequences such as SSFP at 3T. B0 shimming is the standard way to improve the B0 field. However, motion-induced field inhomogeneity is an unknown factor in routine practice and compromises B0 shimming. Here, we adopted a motion-resolved mGRE CMR sequence to investigate the cardiac B0 field perturbation caused by cardiac and respiratory motion. We found that respiratory motion has more impact on field inhomogeneity. We recommend acquiring a field map for shimming under an end-expiration breath-hold for better shimming and imaging at 3T CMR.Introduction
B0-field inhomogeneity has been a long-standing challenge at high-field (3T) CMR. State-of-the-art clinical scanners utilize active B0 shimming, which measures the underlying off-resonance field in the target organ and applies a cancellation shim field to improve B0 homogeneity. This makes the quality of B0 shimming highly dependent on the accuracy of the off-resonance field map measurements1. Due to technical limitations, current cardiac field mapping sequences are commonly acquired with free-running acquisitions that do not consider cardiac or respiratory motion. Since respiratory and cardiac movements alter the geometry of the heart and lungs, it is conceivable that the B0 field can become dependent on the motion state, which can introduce erroneous B0 maps and impede the reliability of B0 shimming for CMR applications. The flawed shim field can induce imaging artifacts and compromise the reliability of B0-sensitive CMR protocols(SSFP). In this study, we utilized a continuously acquired, motion-resolved B0 mapping sequence to investigate the B0 variations during respiratory and cardiac motion. We analyzed the B0 field perturbation in different motion states and proposed a strategy to improve cardiac B0 shimming at 3T.Methods
Healthy volunteers (n=10) were studied with a clinical 3T scanner(Biograph mMR, Siemens Medical Solutions). Continuous 3D, motion-resolved multi-echo GRE (mGRE) data were acquired (6 echoes, TE1/ΔTE =1.42/2.01ms, BW = 640 Hz/pixel, Slice number = 12). mGRE Images were reconstructed with 16 cardiac and 4 respiratory phases based on an LRT CMR framework2. A field map of every motion state is derived and analyzed, as shown in figure 13. In brief, B0 maps derived from the LRT mGRE sequence were unwrapped and corrected for a fat-water chemical shift using the SUPRS algorithm. Subsequently, the calculated phase maps were converted to frequency maps for analysis. For motion-induced field inhomogeneity analysis, the contour of the myocardium was manually drawn in every motion state. Then the region of interest(ROI) was divided into 4 segments(septal, inferior, lateral, and anterior). Frequency variations(FV) (Determined as FV%=RMSE/RMSEExp/Dia - 1) × 100%) were first measured in every segment at every motion state. Then the coefficient of Variance (COV) of FV was determined over the entire myocardium at each motion state. Finally, a paired t-test was used to compare the FV of the whole ROI associated with respiratory and cardiac motion states.Results
Representative motion-resolved B0 field maps from a human subject are shown in Fig.2. Substantial B0 variation was present between inspiration and expiration and remained relatively stable between systole and diastole. Moreover, strong off-resonance variation existed throughout the respiratory cycle in the Field Variation quantification across all respiratory and cardiac motion states(Fig. 3A1 and A2). In contrast, the B0 field remained relatively stable throughout the cardiac cycle. This trend is more predominant in the lateral region than in other segments, where severer off-resonance artifact exists and is more prone to be affected by field inhomogeneity caused by motion. The same trend was evident from the aggregate FV quantification from short-axis view images(Fig. 3 B1 and B2). Field Variation was significantly elevated from inspiration to expiration(p-value = 0.007) but did not change between systole to diastole(p-value = 0.056 > 0.05). COV of FV between end-inspiration and end-expiration is shown in Fig. 3C. Specifically, the B0 field at end-expiration was homogeneous and had the lowest COV across all subjects (p-value < 0.001), supporting the notion that end-expiration is the optimal shimming and imaging state for 3T CMR.Discussion
Breathing motion imparts a significant B0 variation for imaging the heart. Therefore, a consistent respiratory position between B0 mapping and image acquisition is essential for successful cardiac shimming. The developed motion-resolved B0 field maps can provide accurate B0 maps for different motion states and allow correct B0 shimming for CMR acquisitions at 3T. In addition, we found that respiratory motion can cause more field variation compared to cardiac motion. Uncontrolled breathing motion during B0 field acquisition can lead to inaccurate field mapping and results in B0 shim failure with suboptimal CMR images. The Field Variation was particularly significant in the lateral region, which aligns with the region most susceptible to banding artifacts in SSFP images. Based on the discovery, we recommend that field maps for B0 shimming are ideally acquired during an end-expiration breath hold. Moreover, we will soon test our findings and suggestion in patient studies and conduct assessments on improving image quality from the optimized B0 shimming protocol.Conclusions
B0 field varies significantly through the respiratory cycle at 3T while the field stays relatively stable through the cardiac cycle. Based on our findings, we recommend that field maps for shimming are ideally acquired during an end-expiratory breath-hold for breath-held CMR at 3T.Acknowledgements
This work was supported by NIH 1R01HL165211 and NIH R01HL156818References
[1]. H Yang, John Stager, Linda Azab, Waishing Liu, Meng Lu, Yuheng Huang, Ghazal Yoosefian, Skyler Selvin, Richard Handelin, Yujie Shan, Fardad Michael Serry, Yibin Xie, Anthony Christodoulou, Xiaoming Bi, Rohan Dharmakumar, Debiao Li, Hui Han, Whole heart high-order B0 shimming at 3T using a unified coil (UNIC) for RF receive and shimming, Proceedings of the 28th Scientific Annual Meeting of the ISMRM Virtual Meeting(2020) [2]. Xingmin Guan, Hsin-Jung Yang, Zhehao Hu, Nan Wang, Anthony Christodoulou, Behzad Sharif, Debiao Li, Rohan Dharmakumar, Free-breathing, Fully Ungated, 3D Cardiac T2* MR Mapping using a Low-Rank Tensor Framework, 2022 Joint Annual Meeting ISMRM-ESMRMB & ISMRT 31st Annual Meeting (2022) [3]. Dong J, Liu T, Chen F, et al. Simultaneous phase unwrapping and removal of chemical shift (SPURS) using graph cuts: application in quantitative susceptibility mapping. IEEE Trans Med Imaging. 2015;34(2):531-540. doi:10.1109/TMI.2014.2361764Figures
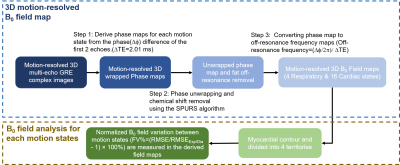
Field map reconstruction and
analysis flow chart: 3D motion-resolved B0 maps were derived
from a continuously acquired mGRE sequence.
After data acquisition, cardiac and respiratory motion-resolved mGRE images2 were used to derive wrapped phase maps. Following, a SPURS3 was used for unwrapping and removing the chemical shift from fat.
Lastly, the processed phase map was converted to 64 field maps (4 respiratory x
16 cardiac states) for field consistency analysis. Finally, the RMSE of the B0 fields in the 4
myocardial territories were measured and compared from each motion
state.
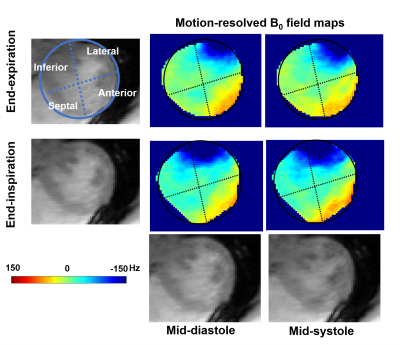
Representative field maps at
different cardiac and respiratory motion states. Representative field maps of the
mid-slice at end-inspiration/end-expiration and mid-systole/mid-diastole are illustrated. Corresponding magnitude images were presented. While the off-resonance field pattern stays consistent
between systole and diastole, significant field variation is presented in the
lateral wall between inspiration and expiration. The off-resonance pattern changes through the respiratory cycle indicate the necessity of
breathing motion mitigation during B0 shimming.
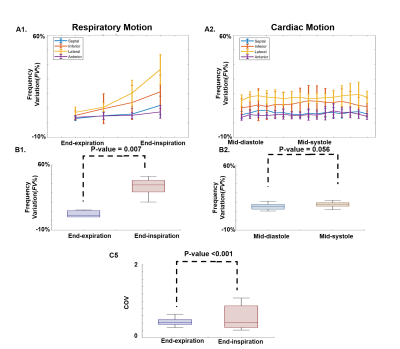
Dependence of Field Variation on respiratory and cardiac motion states. Panel A1 and A2 show representative Frequency Variation(FV) during the respiratory and cardiac cycles. Significantly higher FV is evident throughout the respiratory cycle compared to the cardiac cycle. Panel B shows FV between motion states across all subjects. As observed in panel A, the FV is significantly different between end-inspiration to end expiration but was not different between systole and diastole. Panel C shows the COV of FV between end-inspiration and end-expiration.
DOI: https://doi.org/10.58530/2023/1150