1123
Quantitative T2 Mapping of Articular Cartilage in Patients with Posterior Horn Root Tears of Medial Meniscus1Center for Magnetic Resonance Research, University of Minnesota, Minneapolis, MN, University of Minnesota, Minneapolis, MN, United States, 2Department of Radiology, University of Minnesota, Minneapolis, MN, United States, 3Department of Biomedical Engineering, Lerner Research Institute, Cleveland, OH, United States, 4Twin Cities Orthopedics, Edina, MN, United States, 5Department of Diagnostic and Interventional Radiology, Ataturk University Research Hospital, Erzurum, Turkey
Synopsis
Keywords: Cartilage, Quantitative Imaging
The aim of this study was to evaluate degenerative changes in articular cartilage of patients with posterior root tear of the medial meniscus. Multi-echo quantitative T2 mapping was acquired on a 7T clinical scanner. For reference, age- and gender-matched healthy controls were scanned using the same 7T protocol. Arthroscopic evaluation of articular cartilage and menisci was performed in patients during the repair of posterior medial root tears. Significantly higher T2 values were found in the lateral and medial femoral cartilage of the patients compared to healthy controls.Introduction
Cartilage damage and loss have been associated with meniscal tears1, and meniscal tears are significantly associated with an increased progression of osteoarthritis2. Early identification of degenerative changes in articular cartilage can pave the way to effective treatment plans and potentially avoid or slow-down the progression of knee osteoarthritis3. Ultra-high field 7T provides high resolution and accurate depiction of tissue abnormalities in articular cartilage. The goal of this study was to measure the degenerative changes in articular cartilage of patients with arthroscopically verified posterior medial meniscus root tears.Methods
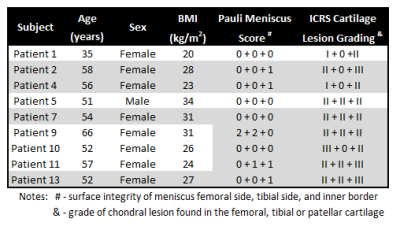
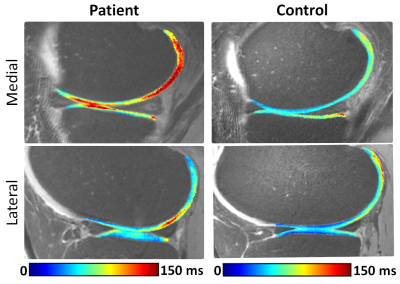
Nine patients with a Type II unilateral posterior root tear of the medial meniscus (mean age, 53 years {age range: 34-66 years}; mean body mass index, 27 kg/m2; 8 women) and seven age-, sex-, and body mass index-matched healthy controls (mean age, 49 years {age range: 34-67}, mean body mass index, 26 kg/m2, 6 women) received 7T MRI and subsequently underwent arthroscopic repair of the root attachment (Fig. 1). The controls had no knee symptoms or abnormal knee MRI findings. Knee MRI was conducted on a 7T system (Siemens, Erlangen, Germany) using a birdcage transmit and 28-channel receive phased-array knee coil. The MRI protocol included T1- and T2-weighted turbo-spin echo sequences with fat suppression for clinical evaluation of the knee joints. For quantitative assessment, a 2D multi-echo spin-echo sequence with five echo times (TE = 13.8, 27.6, 41.4, 55.2, 69 ms) was acquired to measure T2 relaxation times in articular cartilage. The MRI acquisition parameters were: Repetition time (TR)=4080 ms, field of view (FOV)=113x140 mm2, acquisition matrix=352x214, echo train length=5, slice thickness=3 mm, bandwidth=120 Hz/pixel. For the quantitative analysis, T2 maps were calculated by fitting a mono-exponential signal decay of the multi-echo T2 data with two-parametric least-square fitting routine in Matlab. Median T2 values were measured in four regions of articular cartilage including lateral and medial femoral condyles and lateral and medial tibial plateaus on the first or second echoes of T2-weighted images using ITK-SNAP (Fig. 2). Arthroscopic evaluation of articular cartilage and meniscus integrity was carried out during the repair of the posterior root attachment of the medial meniscus. All chondral lesions were classified based on the ICRS grading system4 (Fig. 1). Pauli grading system5 was used to assess the menisci by evaluating the surface integrity of the femoral surface, tibial surface, and inner meniscal surface. For the statistical analyses, a linear mixed effect model, with age and body mass index as covariates, was used to evaluate T2 values between cartilage regions in patients and healthy controls. A P-value of 0.05 was considered as the limit of statistical significance.Results
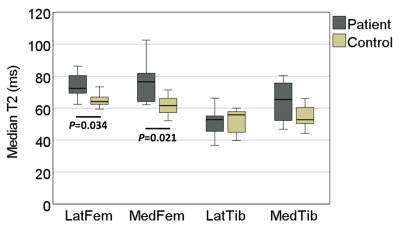
Quantitative T2 maps of a representative patient and a healthy control are shown in Figure 2. Significantly higher T2 values were found (p<0.05) in the medial and lateral femoral articular cartilage of patients compared to the healthy controls (Fig. 3). Arthroscopy evaluation revealed grades I to III cartilage lesions on the femoral, tibial and patellar cartilage (Fig. 1). The medial menisci of all patients had a complete posterior root tear. Based on Pauli grading, five patients had slight to moderate fibrillation at the inner surface, femoral and tibial sides on the medial or lateral menisci. The rest of the menisci surfaces were smooth.Discussion
Elevated T2 values found in the medial and lateral femoral articular cartilage of the patients reveal quantitative measure of chondral abnormalities, which were confirmed by the arthroscopy. The T2 relaxation times were particularly long in the posterior regions of the cartilage situated close to the meniscal root tears. These findings emphasize the role of meniscus in maintaining the integrity of articular cartilage. The results demonstrate the feasibility of T2 mapping of articular cartilage at 7T, which was restricted to 2D multi-slice spin echo imaging due SAR restrictions and long scan time. Further technical development is needed to overcome these challenges to allow a more comprehensive 3D imaging of the cartilage tissue.Conclusion
In vivo T2 mapping at 7T provides a quantitative measure of early degenerative changes in articular cartilage associated with meniscal root tears. Further 7T technical development (e.g. SAR management) and longitudinal follow-up of patients after meniscal repair are needed for this biomarker to reach its potential as a sensitive and accurate investigational tool for disease monitoring and early intervention.Acknowledgements
This study was supported by the NIH-NIBIB grant (P41 EB027061).References
1. Zarins ZA, Bolbos RI, Pialat JB, Link TM, Li X, Souza RB, Majumdar S. Cartilage and meniscus assessment using T1rho and T2 measurements in healthy subjects and patients with osteoarthritis. Osteoarthritis Cartilage. 2010;18(11):1408-16. Epub 20100807. doi: 10.1016/j.joca.2010.07.012. PubMed PMID: 20696262; PMCID: PMC2975868.
2. Floyd ER, Rodriguez AN, Falaas KL, Carlson GB, Chahla J, Geeslin AG, LaPrade RF. The Natural History of Medial Meniscal Root Tears: A Biomechanical and Clinical Case Perspective. Front Bioeng Biotechnol. 2021;9:744065. Epub 2021/10/12. doi: 10.3389/fbioe.2021.744065. PubMed PMID: 34631684; PMCID: PMC8495066.
3. Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonte F, Beaudoin G, Bloch DA, Choquette D, Haraoui B, Altman RD, Hochberg M, Meyer JM, Cline GA, Pelletier JP. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64(4):556-63. Epub 20040916. doi: 10.1136/ard.2004.023796. PubMed PMID: 15374855; PMCID: PMC1755443.
4. Hjelle K, Solheim E, Strand T, Muri R, Brittberg M. Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy. 2002;18(7):730-4. doi: 10.1053/jars.2002.32839. PubMed PMID: 12209430.
5. Pauli C, Grogan SP, Patil S, Otsuki S, Hasegawa A, Koziol J, Lotz MK, D'Lima DD. Macroscopic and histopathologic analysis of human knee menisci in aging and osteoarthritis. Osteoarthritis Cartilage. 2011;19(9):1132-41. Epub 2011/06/21. doi: 10.1016/j.joca.2011.05.008. PubMed PMID: 21683797; PMCID: PMC3217905.
Figures