1074
DIRECT: non-contrast-enhanced relaxation-based flow-independent intracranial MR angiography using modified REACT1Philips Japan, Tokyo, Japan, 2Department of Radiology, Eastern Chiba Medical Center, Chiba, Japan, 3Department of Radiological Services, Tokyo Women's Medical University, Tokyo, Japan, 4Department of Diagnostic Imaging and Nuclear Medicine, Tokyo Women’s Medical University, Tokyo, Japan, 5Philips Healthcare, Hamburg, Germany, 6Philips Healthcare, Best, Netherlands
Synopsis
Keywords: Vessels, Blood vessels
A new non-contrast-enhanced, relaxation-based, flow-independent MRA method, called Relaxation-Enhanced Angiography without ContrasT (REACT) has recently been proposed for vascular imaging. One of the major limitations of REACT is that bright signal of long-T1 fluids such as CSF is visible, which can obscure vascular structure in the intracranial vessels. We developed a new sequence, called DIRECT (Dual-Inversion REaCT) with modified magnetization preparation scheme of REACT to suppress CSF signals while maintain the high signal intensity from vessels. DIRECT enables robust and high-quality whole-brain intracranial MR angiography with uniform fat, CSF and brain parenchyma suppression within clinically feasible scan time.Introduction
A new non-contrast-enhanced, relaxation-based, flow-independent MRA method, called Relaxation-Enhanced Angiography without ContrasT (REACT) has recently been proposed for vascular imaging in various body parts with large anatomical coverage1,2. REACT consists of a 3D dual-echo Dixon segmented gradient echo and magnetization preparation using a T2prep pulse and a non-selective inversion recovery (IR) pre-pulse to emphasize the blood signals while suppressing background signals.REACT has been clinically adapted to a wide range of areas, including evaluation of pediatric vascular diseases, vessels in acute stroke, renal artery stenosis, and vascular malformations3-7. In addition, because REACT depicts not only arteries but also veins, it has been reported to be useful in detecting venous lesions such as deep vein thrombus and in evaluating central veins and brachial veins in patients with end-stage renal failure before starting dialysis7,8.
One of the major limitations of REACT is that bright signal of long-T1 fluid, such as cerebrospinal fluid (CSF) is visible, which can obscure vascular structure particularly in the intracranial vessels1. An improved suppression of this long-T1 CSF signal is clinically desirable especially for pediatric patients. To solve this problem, we attempted to develop a new sequence, called DIRECT (Dual-Inversion REaCT) with modified magnetization preparation scheme of REACT to suppress CSF signals while maintain the high signal intensity from blood vessels. The purpose of this study is to evaluate the feasibility of DIRECT in visualization of intracranial vessels.
Methods
DIRECT sequence:A schematic overview of the DIRECT sequence is shown in Figure 1. It basically consists of a signal readout by 3D Dixon dual-echo turbo field-echo (TFE) preceded by dual non-selective inversion recovery (IR) pulses, instead of T2 prepararion pulse and IR combination, which is applied in the original REACT implementation. Magnetization preparation pulses were implemented to suppress signal from tissues especially for brain parenchyma and CSF, according to their difference in T1 relaxation times. In detail, a first IR pulse was applied with a long inversion time (TI) followed by a second IR pulse with relatively shorter TI to suppress tissues with intermediate-to-long T1 relaxation times, thus enhancing the blood-to-tissue contrast during the signal readout while suppressing the CSF signals. On the other hand, fat signals can be suppressed by DIXON water-fat separation. Besides, for robustness against B1 and B0 sensitivity across the entire the FOV, we applied a broadband inversion pulse for dual-IR pulses, as already introduced for spine MR bone-weighted imaging9,10.
Experiments:
A total of seven volunteers were examined on a 3.0T whole-body clinical system (Ingenia/Ingenia CX, Philips Healthcare). The study was approved by the local IRB, and written informed consent was obtained from all subjects.
DIRECT images were compared with conventional 3D Time-of-flight (TOF) MRA and conventional REACT images for image quality, especially for the overall SNR and the contrast between vessels and background signals.
Imaging parameters for DIRECT were; Sagittal, voxel size=1.20x1.20 x1.20mm3, TFE shot-interval=3000ms, Inversion Delay (TI) 1/2=1900/400ms, TR=3.9ms, TE1/TE2=1.3/2.3ms, flip angle=12°, NSA=1, TFE factor=50, Compressed SENSE-reduction factor=2.8, and total acquisition time=5m44s. Parameters for REACT were; Sagittal, voxel size=1.20x1.20 x1.20mm3, TFE shot-interval=3000ms, Inversion Delay (TI) =100ms, T2prep pulse with duration of 50ms, TR=3.9ms, TE1/TE2=1.3/2.3ms, flip angle=12°, NSA=1, TFE factor=50, Compressed SENSE-reduction factor=2.8, and total acquisition time=5m44s. Parameters for TOF-MRA were; Axial, voxel size=1.0x1.0 x1.0mm3, TR=23ms, TE =3.45ms, flip angle=18°, NSA=1, Compressed SENSE-reduction factor=4.5 and total acquisition time=6m32s.
Results and Discussion
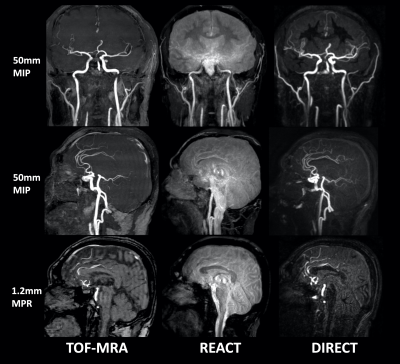
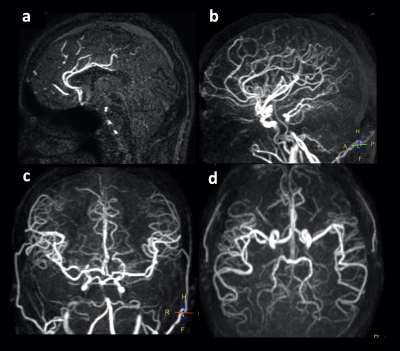
The quality of DIRECT MRA was considered comparable to that of the conventional TOF-MRA whereas conventional REACT did not depict intracranial vessels well. Representative images including different image post-processing from all these techniques are shown in Figure 2. It is noteworthy that DIRECT provided intracranial MRA with sufficient contrast between arteries and background signals including fat, CSF and brain parenchyma (both white matter and grey matter) and allowed for imaging over whole-brain at 3.0T.Figure 3 shows representative DIRECT images in another subject compared to the TOF-MRA. DIRECT clearly showed the intracranial arteries as well as TOF-MRA without use of saturation pulse. Although further clinical investigation is needed, this technique can provide comparable information with TOF-MRA sequence. Figure 4 also shows representative DIRECT MRA with orthogonal MIP images in addition to source image. The anatomical information of the intracranial blood vessels provided was at least visually equivalent to that obtained from the conventional sequence. It may even be superior owing to uniform background tissue suppression thanks to optimized dual inversion delays, the efficacy of which would need to be investigated more systematically.
Conclusion
DIRECT enables robust and high-quality whole-brain intracranial MR angiography with uniform fat, CSF and brain parenchyma suppression within clinically feasible scan time. It holds promise for assessment of cerebrovascular diseases and further clinical studies in comparison to the other state-of-the-art methods are needed.Acknowledgements
No acknowledgement found.References
1. Yoneyama M, et al. Free-breathing non-contrast-enhanced flow-independent MR angiography using magnetization-prepared 3D non-balanced dual-echo Dixon method: A feasibility study at 3 Tesla. Magn Reson Imaging. 2019:16;63:137-146.
2. Nair PP, et al. iREACT: A Non-contrast Non-triggered MR Angiography Technique with Reduced RF Deposition. Applied Magnetic Resonance. 2022;53:335-342.
3. Dillman JR, et al. Non-contrast three-dimensional gradient recalled echo Dixon-based magnetic resonance angiography/venography in children. Pediatr Radiol. 2019;49:407-414.
4. Pennig L, et al. Imaging of the pulmonary vasculature in congenital heart disease without gadolinium contrast: Intraindividual comparison of a novel Compressed SENSE accelerated 3D modified REACT with 4D contrast-enhanced magnetic resonance angiography. J Cardiovasc Magn Reson. 2020;22:8.
5. Isaak A, et al. Free-breathing non-contrast flow-independent cardiovascular magnetic resonance angiography using cardiac gated, magnetization-prepared 3D Dixon method: assessment of thoracic vasculature in congenital heart disease. J Cardiovasc Magn Reson. 2021;23:91.
6. Pennig L, et al. Relaxation-enhanced angiography without contrast and triggering (REACT) for fast imaging of extracranial arteries in acute ischemic stroke at 3T. Clin Neuroradiol. 2020;31:815–826.
7. Tan EJ, et al. REACT – A novel flow-independent non-gated non-contrast MR angiography technique using magnetization-prepared 3D non-balanced dual-echo dixon method: Preliminary clinical experience. Eur J Radiol Open. 2020;7:100238.
8. Terwolbeck MN, et al. Relaxation-Enhanced Angiography without Contrast and Triggering (REACT) for pelvic MR venography in comparison to balanced gradient-echo and T2-weighted spin-echo techniques. Clin Imaging. 2021;74:149-155.
9. Yoneyama M, et al. Robust motion-compensated lumbar spine bone imaging using 3D UTE with broadband inversion recovery pulse and k-space weighted navigator gating. Proc Intl Soc Mag Reson Med. 2019;27:0133.
10. Yoneyama M, et al. 3D broadband IR-prepared UTE bone imaging for assessment of ossification of the posterior longitudinal ligament (OPLL) in the cervical spine. Proc Intl Soc Mag Reson Med. 2019;27:2873.
Figures
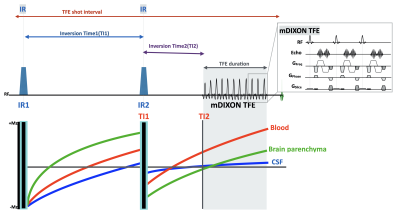
Figure 1. Scheme overview of DIRECT sequence.
DIRECT consisting of a signal readout by 3D Dixon dual-echo turbo field-echo (TFE) preceded by dual non-selective IR pulses. A first IR pulse was applied with a long inversion time (TI) followed by a second IR pulse with relatively shorter TI to suppress brain parenchyma and CSF, thus enhancing the blood-to-tissue contrast during the signal readout for intracranial MRA. Besides, for robustness against B1 and B0 sensitivity across the entire the FOV, we applied a broadband IR pulse for dual-IR pulses.