0981
Intelligent Slice Placement for Oblique Coronal ACL plane prescription for Knee MRI using Deep Learning
Apoorva Agarwal1, Chitresh Bhushan2, Desmond T.B. Yeo2, Thomas Foo2, Dawei Gui3, Deepa Anand1, Maggie Fung4, Trevor Kolupar3, Tisha Abraham1, Sanjay NT1, Kameswari Padmanabhan1, Uday Patil1, and Dattesh Shanbhag1
1GE Healthcare, Bengaluru, India, 2GE Global Research, Niskayuna, NY, United States, 3GE Healthcare, Waukesha, WI, United States, 4GE Healthcare, New York City, NY, United States
1GE Healthcare, Bengaluru, India, 2GE Global Research, Niskayuna, NY, United States, 3GE Healthcare, Waukesha, WI, United States, 4GE Healthcare, New York City, NY, United States
Synopsis
Keywords: Machine Learning/Artificial Intelligence, MSK
In clinical practice, oblique coronal and sagittal scans have been shown to be superior for visualization of ACL and assessment of ACL tears. In this work, we demonstrate a Deep Learning based method to obtain these complex scan planes (Coronal ACL and Coronal Blumensaat) directly from standard 2D tri-planar Localizers. Results on 487 test volumes show <0.6mm mean error for both planes, indicating suitability for clinical usage.Summary of Main Findings
A Deep Learning (DL) model adapted for Coronal Knee MR prescription on standard 2D tri-planar Localizer images for ACL and Blumensaat Line was obtained with mean error < 0.6mm. Results indicate suitability for clinical usage of ACL prescription.Introduction
Oblique coronal ACL imaging in addition to oblique sagittal knee plane is used for improving the diagnostic accuracy of detecting single/double bundle injury of ACL1 and improving detection of partial/complete ACL tears2,3. As ACL has fine anatomy (thickness < 5mm), precise angulation is challenging and requires highly skilled technicians in clinical practice4. In this work, we present an Intelligent Slice Placement (ISP) framework using standard 2D tri-planar Localizer images that allows for contiguous visualization of ACL, irrespective of changes in patient position, minor anatomical changes, and technologist training. Previous efforts to automate prescription include use of specialized 3D localizers and landmark detection, or more recently, use of DL-based generalized framework for MRI scan plane prescription5,6. In this work, we have adapted the previously described generic ISP framework for Brain6 and Knee7 with only training data and plane definitions adapted for ACL in the oblique coronal plane.Traditional algorithms use high-resolution data to visualize, segment and generate ACL plane prescription as ACL is not easily visualized in standard low-resolution 2D Localizers. Algorithms that rely on explicit ACL computation from high-resolution data produce inaccurate results in cases where ACL is torn, attenuated, or obscured by artifacts from metal implants. The clinically accepted alternative in such scenarios is to use the bone-centric Blumensaat Line as a surrogate for ACL plane8.
In our work, we use a DL network to predict ACL plane and Blumensaat Line from standard Localizer images without explicit segmentation of the structures by predicting the scan plane masks. Even when the integrity of ACL is not preserved or the structure is not visible, we hypothesize that the DL network is able to learn the entire 3-dimensionalanatomical context and produce robust plane predictions. Our DL models simultaneously predict both ACL and Blumensaat planes and hence allow both options for oblique coronal ACL prescription based on clinician preferences.
Methods
Subjects: Knee MRI data for study came from multiple sites. A total of 1306 knee exams from volunteers as well as patients were included in the study. All the studies were approved by respective Institutional Review Boards.MRI Scanner and Data Acquisition: Localizer Data was acquired on multiple MRI scanners (GE 3T Discovery MR 750w, GE Signa HDxt 1.5T, GE 1.5T Optima 450w) and with different coil configurations (e.g.,16-/ 18-channel TR Knee coil, GEM Flex coil etc.). Localizer data varied in contrast (FGRE, SSFSE), image resolution, field of view, slice coverage and matrix size across subjects.
DL Methodology: Ground-truth (GT) landmark points were marked by a trained radiologist and then translated into imaging planes for DL segmentation. Two points each were marked on the ACL and Blumensaat Line to generate the tilt of oblique coronal planes (Fig.1). A total of 1062 exams (30,652 volumes after augmentation) were used for training/validation and 258 exams (487 volumes after augmentation) were used for testing. A variety of Intensity and Geometry augmentations were applied. Multi-task Learning was used to train single segmentation model that infers on sagittal Localizer images to output two segmentation plane masks – one each for ACL and Blumensaat Line (Fig.2).
Accuracy Assessment: Accuracy was assessed by calculating mean absolute distance (MAD) error and angle error between GT and DL predictions for both planes. MAD error < 1 mm and angle-error < 4⁰ was considered as acceptable for ISP.
Results and Discussion
Mean MAD error obtained was 0.55mm for ACL plane and 0.48mm for Blumensaat Line plane predictions on test cohort of 487 datasets on comparison with GT (Fig.3). Apart from clinically normal cases, the test cohort also contained Localizers that include pediatric, geriatric cases, fractured knees, osteotomies, pathologies, and metal implants. MAD errors for selective subset of the test cohort that include the above are as shown in Fig.3.The model provided robust plane predictions, even in presence of metal (Fig.4) and torn/obscured ACL (Fig.5). Effectiveness of our ISP framework is demonstrated in a prospective reformatting of high-resolution isotropic CUBE T2-weighted knee using predicted planes (Fig.5), which indicates contiguous visualization of ACL.
Conclusion
We have adapted a generalized DL-based intelligent slice placement framework for predicting the oblique coronal planes along ACL and Blumensaat Line. The results indicate that the framework allows for successful oblique coronal ACL prescription with <0.6mm error and <4 degrees error. Results demonstrate its clinical readiness with robust performance even in presence of artifacts in the Localizer data. Bone-based Blumensaat Line landmark can be successfully used as surrogate for ACL, in cases with severe ACL injury (torn, attenuated) or obscured ACL.Acknowledgements
No acknowledgement found.References
- Yasser I. Abd Elkhalek, M.D, Moustafa Abdel Kawi, M.D. and Merhan Nasr, M.Sc. Combining ACL Oblique Coronal MRI with the Routine Knee MRI Protocol in the Diagnosis of ACL Bundle Lesions. Can It Add A Value? Med. J. Cairo Univ., Vol. 87, No. 7, December: 4795-4801, 2019.
- Soliman, H.H. Concurrent use of oblique sagittal and oblique coronal MRI: does it enhance the specificity and the accuracy of diagnosing complete and partial ACL tears? Egypt J Radiol Nucl Med 51, 22 (2020).
- Hong, Sung Hwan MD; Choi, Ja-Young MD; Lee, Gyung Kyu MD; Choi, Jung-Ah MD; Chung, Hye Won MD; Kang, Heung Sik MD. Grading of Anterior Cruciate Ligament Injury: Diagnostic Efficacy of Oblique Coronal Magnetic Resonance Imaging of the Knee. Journal of Computer Assisted Tomography: September 2003 - Volume 27 - Issue 5 - p 814-819.
- Martin J. Breitenseher, MD and Marius E. Mayerhoefer, MD. Oblique MR Imaging of the Anterior Cruciate Ligament Based on Three-Dimensional Orientation. Journal Of Magnetic Resonance Imaging 26:794 –798 (2007).
- Lecouvet FE, Claus J, Schmitz P, Denolin V, Bos C, Vande Berg BC. Clinical evaluation of automated scan prescription of knee MR images. Journal of Magnetic Resonance Imaging: An Official Journal of the International Society for Magnetic Resonance in Medicine. 2009 Jan; 29(1):141-5.
- Shanbhag DD et.al. A generalized deep learning framework for multi-landmark intelligent slice placement using standard tri-planar 2D localizers. In Proceedings of ISMRM 2019, Montreal, Canada, p. 670.
- Bhushan et al., Intelligent Knee MRI slice placement by adapting a generalized deep learning framework, ISMRM & SMRT Virtual Conference & Exhibition, p. 3562, (2020).
- Arthur B. Meyers, et al. Imaging of Anterior Cruciate Ligament Repair and Its Complications. AJR:194, February 2010.
Figures
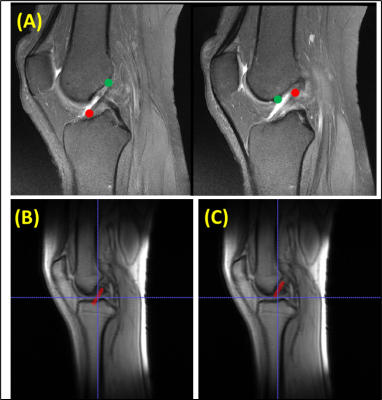
Figure 1: Illustration of Ground Truth (GT) for our ISP framework. (A) High-resolution images are
marked by radiologist to different planes: Anterior Cruciate Ligament (ACL) in
red and Blumensaat Line in blue. Note that marking may extend beyond one slice.
For Deep Learning training, these are translated as plane mask on corresponding
tri-planar 2D Localizer for (B) ACL and (C) Blumensaat Line.
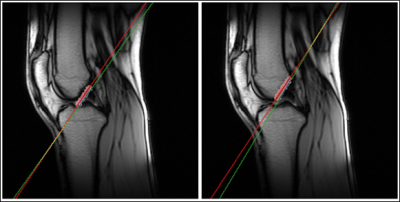
Figure 2: Example of prediction from our Multi-task
trained DL model for (Left) ACL prediction and (Right) Blumensaat Line. GT plane
is shown in green and DL-estimated plane is shown in red. (DL-predicted
segmentation is shown as a red blob). Small angle between GT (red) and
predicted (green) planes indicates excellent accuracy of our DL model.
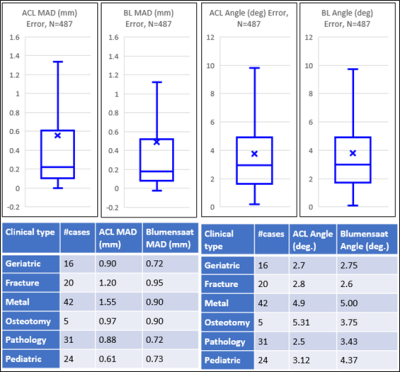
Figure 3: Box plots (top-row) show summary of
errors in ISP as compared to Ground Truth for ACL and Blumensaat Line. MAD
error < 0.6mm and Angle error < 4 degrees obtained
for ACL and Blumensaat Line both on comparison with GT. MAD and Angle errors
for subset of test data (bottom-row) demonstrates errors across data of varied
clinical types.
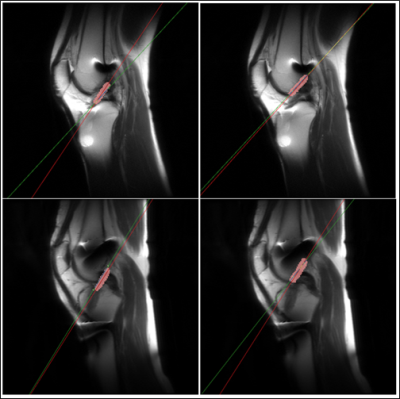
Figure 4: Illustration of robust performance in
presence of metal implants in two patients (row-wise) for (left) ACL prediction
and (right) Blumensaat Line. GT plane is shown in green and DL-estimated plane
is shown in red. (DL-predicted segmentation is shown as a red blob). Small
angle between GT (red) and predicted (green) planes indicates good accuracy of
our DL model.
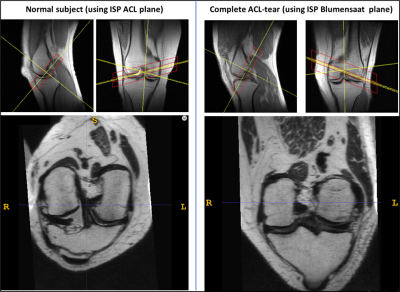
Figure 5: Examples of ISP predicted scan planes and
retrospective reformatting of 3D isotropic T2-w data using predicted planes for (left) a typical, normal subject, and (right) a case
with complete ACL tear. For each case, top row images show scan plane prediction
overlaid on top of Localizer image and bottom row image shows reformatted view
of high-resolution isotropic CUBE T2-weighted knee using predicted planes. Note
that in case with complete ACL tear, Blumensaat Line was successfully used for
reformatting.
DOI: https://doi.org/10.58530/2023/0981