0797
Incorporating diffusion weighted MRI into a radiomics model improves diagnostic performance in survival prediction in PDAC
Piaoe Zeng1, Jingjing Cui2, and Huihui Yuan3
1radiology, peking university third hospital, Beijing, China, 2United Imaging Intelligence (Beijing), Beijing, China, 3Peking university third hospital, Beijing, China
1radiology, peking university third hospital, Beijing, China, 2United Imaging Intelligence (Beijing), Beijing, China, 3Peking university third hospital, Beijing, China
Synopsis
Keywords: Pancreas, Cancer, magnetic resonance imaging; radiomics;
Radiomics features were extracted from multiparametric MRI including conventional MRI (T2WI, T1WI, arterial phase, portal venous phase images) and apparent diffusion coefficient (ADC). The radiomics score was built based on the least absolute shrinkage and selection operator regression model. Three models, including clinicopathological and radiographic characteristics (CPR) model, multiparametric MRI radiomics model and conventional MRI radiomics model, were built to predict recurrence-free survival (RFS) and overall survival (OS) in patients with resectable pancreatic ductal adenocarcinoma (PDAC). Multiparametric MRI radiomics model showed improved diagnostic performance in survival prediction than conventional MRI radiomics model and CPR model.Background or Purpose
Establishing a risk stratification of pancreatic adenocarcinoma (PDAC) is necessary before treatment, which could predict postsurgical recurrence-free time interval as well as life expectancy and provide more efficient individualized treatment strategy by implementing neoadjuvant, extended surgical resection and adjuvant therapy to reduce the risk of local tumor recurrence or distant metastasis, thereby prolonging survival. The current methods used to predict the prognosis of PDAC are mainly through pathology and imaging. In addition to the established clinical prognostic factors, radiomics has attracted increasing attention in predicting tumor prognosis in the last few years. Previous studies have shown that radiomics models based on computed tomography (CT) images have the potential to predict recurrence and overall survival in patients with PDAC. However, the utilization of diffusion-weighted imaging (DWI) has been limited in radiomics analysis. As DWI–derived apparent diffusion coefficient (ADC) value reflects tumor characteristics, we hypothesized that incorporating them into a radiomics model would provide better prediction of survival in PDAC. The purpose of this study was, therefore, to determine whether radiomics features obtained from DWI MRI could help predicting survival in PDAC, and to further determine how they compare with a conventional MRI radiomics model and a clinicopathological and radiographic characteristics (CPR) model.Methods
193 patients with PDAC from January 2012 to June 2021 were included retrospectively and were randomly divided into training and validation sets at a ratio of 7:3. Radiomics features were extracted from T2-weighted imaging(T2WI), T1-weighted imaging(T1WI), arterial phase (AP), portal venous phase images (PVP) and apparent diffusion coefficient (ADC) maps drived from DWI, respectively. Overall, 1,094 radiomics features were extracted from each volume of interest drawn. The radiomics score was built based on the least absolute shrinkage and selection operator regression model. The radiomics score was converted into high-risk or low-risk groups with the cut-offs. A multiparametric MRI radiomics model (based on T2WI, T1WI, AP, PVP and ADC images) and a conventional MRI radiomics model (based on T2WI, T1WI, AP, PVP images) were built. In addition, the clinicopathological data and radiographic characteristics were collected and a clinicopathological and radiographic characteristics (CPR) model was built. The performances of the above three models were evaluated by concordance index (C-index), calibration curve, and decision curve analysis (DCA). The Integrated discrimination improvement (IDI) was used to quantify the improvement of prognostic accuracy in multiparameter MRI radiomics model over the CPR model and the conventional MRI radiomics model.Result
Results: The high-risk patients defined by the radiomic score showed significantly lower RFS and OS compared with low-risk patients in validation set. The multiparametric MRI radiomics model showed the significantly better performance in predicting RFS than the CPR model (C-index 0.792 vs. 0.711, P<0.001, IDI improvement 22.7%) and conventional MRI radiomics model (C-index=0.792 vs.0.710, P=0.006, IDI improvement 22.7%) and predicting OS than the CPR model (C-index=0.764 vs.0.701, P=0.002, IDI improvement 15.7%) and conventional MRI radiomics model (C-index=0.764 vs.0.710, P=0.023, IDI improvement 15.9%) in the validation set. Decision curve analysis demonstrated that in terms of clinical usefulness, the multiparametric MRI radiomics model outperformed the conventional MRI radiomics model and the CPR model.Conclusions
Multiparametric MRI radiomics model showed improved diagnostic performance in survival prediction than conventional MRI radiomics model and CPR model, with ADC features playing a significant role.Acknowledgements
No acknowledgement foundReferences
1. Chun YS, Pawlik TM, Vauthey JN. 8th Edition of the AJCC Cancer Staging Manual: Pancreas and Hepatobiliary Cancers. Ann Surg Oncol 2018;25:845-847. 2. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-249. 3. Allen PJ, Kuk D, Castillo CF, et al. Multi-institutional Validation Study of the American Joint Commission on Cancer (8th Edition) Changes for T and N Staging in Patients With Pancreatic Adenocarcinoma. Ann Surg 2017;265:185-191. 4. Huang, Y., et al., Radiomics Signature: A Potential Biomarker for the Prediction of Disease-Free Survival in Early-Stage (I or II) Non-Small Cell Lung Cancer. Radiology, 2016. 281(3): 947-957. 5. Chu, F., et al., Development and validation of MRI-based radiomics signatures models for prediction of disease-free survival and overall survival in patients with esophageal squamous cell carcinoma. Eur Radiol, 2022. 6.Yang, Y., et al., Multiparametric MRI-Based Radiomic Signature for Preoperative Evaluation of Overall Survival in Intrahepatic Cholangiocarcinoma After Partial Hepatectomy. J Magn Reson Imaging, 2022. 56(3): 739-751. 7. Tang, T.Y., et al., Development of a Novel Multiparametric MRI Radiomic Nomogram for Preoperative Evaluation of Early Recurrence in Resectable Pancreatic Cancer. J Magn Reson Imaging, 2020. 52(1): p. 231-245. 8. Xie, T., et al., Pancreatic ductal adenocarcinoma: a radiomics nomogram outperforms clinical model and TNM staging for survival estimation after curative resection. Eur Radiol, 2020. 30(5): 2513-2524. 9. Kim, M., et al., Diffusion- and perfusion-weighted MRI radiomics model may predict isocitrate dehydrogenase (IDH) mutation and tumor aggressiveness in diffuse lower grade glioma. Eur Radiol, 2020. 30(4): 2142-2151. 10. Kim, D.W., et al., Estimating Recurrence after Upfront Surgery in Patients with Resectable Pancreatic Ductal Adenocarcinoma by Using Pancreatic CT: Development and Validation of a Risk Score. Radiology, 2020. 296(3): 541-551. 11. Salinas-Miranda, E., et al., Prognostic value of early changes in CT-measured body composition in patients receiving chemotherapy for unresectable pancreatic cancer. Eur Radiol, 2021. 31(11): 8662-8670. 12. Cassinotto, C., et al., Pancreatic adenocarcinoma: A simple CT score for predicting margin-positive resection in patients with resectable disease. Eur J Radiol, 2017. 95: 33-38. 13. Zaky, A.M., et al., Tumor-Vessel Relationships in Pancreatic Ductal Adenocarcinoma at Multidetector CT: Different Classification Systems and Their Influence on Treatment Planning. Radiographics, 2017. 37(1): 93-112. 14. Chang, S.T., et al., Preoperative Multidetector CT Diagnosis of Extrapancreatic Perineural or Duodenal Invasion Is Associated with Reduced Postoperative Survival after Pancreaticoduodenectomy for Pancreatic Adenocarcinoma: Preliminary Experience and Implications for Patient Care. Radiology, 2016. 281(3): 816-825. 15. Al-Hawary, M.M., et al., Pancreatic ductal adenocarcinoma radiology reporting template: consensus statement of the Society of Abdominal Radiology and the American Pancreatic Association. Radiology, 2014. 270(1): 248-60.Figures
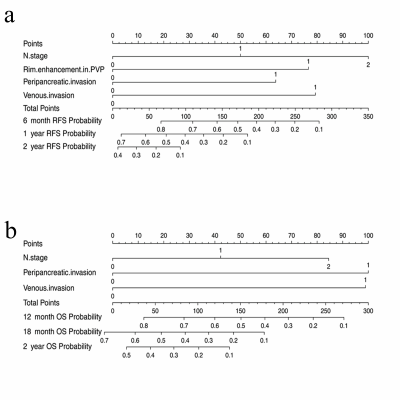
Figure 1:CPR nomogram models for predicting RFS and OS. The nomogram wasdeveloped for DFS (a) and OS (b).
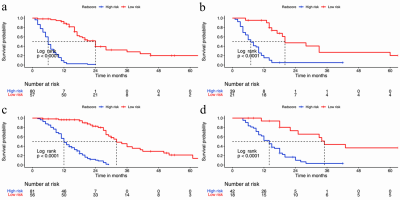
Kaplan–Meier estimates of RFS(a,b) and OS(c,d) for patients stratified by conventional MRI radiomics score in the training set (a, c) and validation set (b, d).
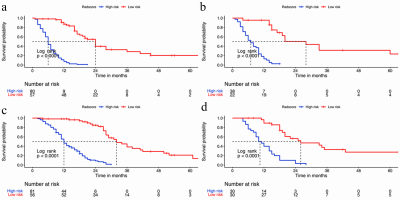
Kaplan–Meier estimates of RFS(a,b) and OS(c,d) for patients stratified by multiparameter MRI radiomics score in the training set (a, c) and validation set (b, d).

Calibration curves of the CPR model(a,d), conventional MRI radiomics model (b,e)and multiparameter MRI radiomics model (c,f) in predicting RFS(a,b,c) and OS(d,e,f).
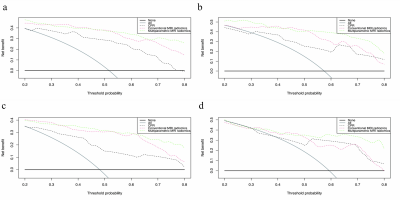
Decision curve analysis for the CPR model, conventional MRI radiomics model and multiparameter MRI radiomics model. in the training (a,c) and validation set (b, d), to predict RFS(a,b) and OS(c,d).
DOI: https://doi.org/10.58530/2023/0797