0796
Long-term evolution of liver imaging reporting and Data system Version 2018 category 2, 3, and 4 observations on MRI in HBV-related cirrhosis1the Third Affiliated Nantong Hospital of Nantong University, Nantong, China, 2Philips Healthcare, Beijing, China, 3Philips Healthcare, Shanghai, China
Synopsis
Keywords: Liver, Cancer, HCC
This study assessed the imaging outcomes of Liver Imaging Reporting and Data System (LI-RADS) v2018 category 2, 3, and 4 observations in prospective hepatocellular carcinoma (HCC) surveillance cohort. LI-RADS observations demonstrate increasing risk of progression to HCC with increasing category. About two-fifths of LR-4 progressed to a malignant category. LR-3 observations with APHE or threshold/subthreshold growth upgraded to LR-5 were significantly higher. Most LR-2 observations that remain stable in category for at least two years.Introduction
Hepatocellular carcinoma (HCC) is regarded as the sixth most commonly diagnosed cancer and the fourth most common cause of cancer-related deaths worldwide, particularly for HCC patients with hepatitis B1. HCC surveillance is associated with improved early detection, curative treatment receipt, and survival. Imaging modalities play a crucial role in the diagnosis and staging of HCC, especially for MR imaging, which is widely used for the diagnosis of HCC due to its high tissue contrast and depiction of major imaging features of HCCs2, 3.Liver Imaging Reporting and Data System (LI-RADS, LR) is a comprehensive system for standardizing the terminology, interpretation, reporting, and data collection of liver observations in at-risk individuals, ranging from LR-1 (“definitely benign”) to LR-5 (“definitely HCC”). Indeterminate observations are classified into three distinct categories: LR-2 (probably benign), LR-3 (intermediate probability for malignancy), and LR-4 (probably HCC), with a baseline risk of 13% (95%CI 8%-22%), 38% (95%CI 31%-45%), and 74% (95%CI 67%-80%) of being HCC, respectively4, 5. Although several previous studies have reported on the outcomes of observations classified according to LI-RADS categories, they are limited by standardized imaging techniques (i.e. different follow-up imaging tests including CT and MRI), assessed longitudinal clinical outcomes with previous versions of LI-RADS (i.e. v2014 or v2017), and few LR-2 observations progressed to LR-56. Recently, several studies reported the longitudinal evaluation of LR-2, LR-3, or LR-4 observations using LI-RADS v2018, but risk estimates remain imprecise (i.e. the probability of LR-3 observations progressing to LR-5 or LR-M being 11.1% vs. 44.4%)7,8. Therefore, this study aimed to retrospectively analyze, by using LI-RADS v2018, the natural outcomes of LR-2, LR-3, and LR-4 observations on serial MRI surveillance, including incidence and mean time to a higher LI-RADS categories, and to identify predictors of progression to LR-5 or higher.Methods
Data from 158 patients(213 observations)of cirrhosis who underwent at least one follow-up magnetic resonance imaging (MRI) examination in our institution from September 2016 to October 2022, and were index category as LR-2, LR-3 and LR-4 lesions without biopsy or operation,were retrospectively reviewed. Among all the observations, 74 were LR-2, 95 were LR-3 and 44 were LR-4. Follow-up duration and category modifications that progressed, remained stable, or decreased were recorded for each observation. The single-factor analysis was used to analyze the follow-up interval of LR-2, LR-3 and LR-4 observations, and cumulative incidence curves for progression were analyzed. All statistical analyses were performed on a per-observation basis using SPSS version 26.0 and R version 4.2.0Results
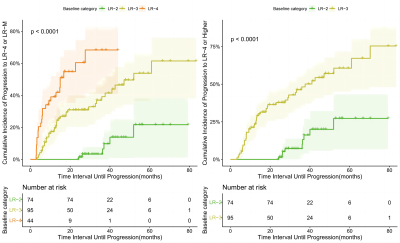
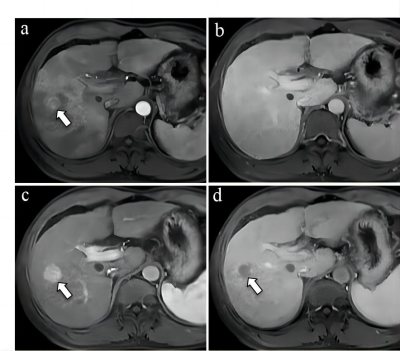
The mean follow-up interval of LR-2, LR-3 and LR-4 were(20.5±11.4),(18.1±10.5)and(13.8±9.9) months respectively, the difference were statistically significant(F=6.58, P=0.002). Among 74 index LR-2 observations, 5 upgraded to LR-5, 2 upgraded to LR-4, 4 upgraded to LR-3, 63 remained stable or decreased. Among 95 index LR-3 observations, 17 upgraded to LR-5, 6 upgraded to LR-4, 57 remained stable and 15 decreased to LR-1/-2. Among 44 index LR-4 observations, 15 upgraded to LR-5, among them, 5 demonstrated threshold growth, 7 demonstrated subthreshold growth; 2 progressed to LR-TIV with venous invasion, 23 remained stable and 3 decreased to LR-1. The cumulative incidence of progression to LR-5/-TIV was higher for LR-4 observations than for LR-3 or LR-2 observations (each P<.001). Among them, the cumulative incidence of upgraded to LR-5 in 3, 6, and 12 months, LR-4 lesions were 4.7%、11.6%、31.2%, LR-3 lesions were 0、4.2%、6.6%, respectively, and LR-2 lesions were 0. The cumulative incidence of progression to LR≥4 was higher for LR-3 lesions than for LR-2 lesions (P<.001).Discussion
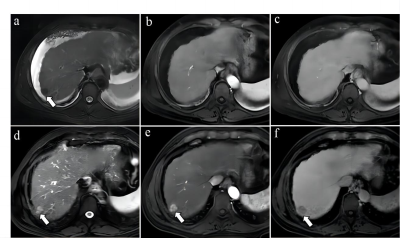
This study demonstrates that LR-2, LR-3, and LR-4 observations have significantly different long-term imaging outcomes by using LI-RADS v2018. LR-2, LR-3, and LR-4 have an increasing likelihood of progression to malignant categories(LR-5 or LR-TIV): in particular, LR-2 observations have a cumulative incidence of progression to LR-5 of 0%, 0%, 0%, and 3.6% at 3 months, 6 months, 1 year, and 2 years, respectively; LR-3 observations have a cumulative incidence of progression to LR-5 of 0%, 4%, 9%, and 23%; and LR-4 observations have a cumulative incidence of progression to LR-5 of 5%, 12%, 31%, and 63%. In this study, LR-2 observations were all homogeneous cirrhotic siderotic nodules(SN) that have no ancillary features(AF) malignancy, 6.8% (5/74) LR-2 SN progressed to LR-5, 9.5% (7/74) of LR-2 SN upgrade to probable or definite HCC. Iron clearance, hyperintense on T2WI and hypervascular transformation elevation on the follow-up MRI indicated the multistep hepatocarcinogenesis. These results indicate that the LI-RADS categorization can provide reliable information for management decisions, as well as stratify patients according to the risk of progression.Conclusion
Observations classified according to LI-RADS version 2018 categories are associated with different imaging outcomes.Acknowledgements
No acknowledgement found.References
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries [published correction appears in CA Cancer J Clin. 2020 Jul;70(4):313]. CA Cancer J Clin. 2018;68(6):394-424.
2. Vitale A, Trevisani F, Farinati F, et al. Treatment of Hepatocellular Carcinoma in the Precision Medicine Era: From Treatment Stage Migration to Therapeutic Hierarchy. Hepatology. 2020;72(6):2206-2218.
3. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723-750.
4. Kim YY, Choi JY, Kim SU, et al. MRI ancillary features for LI-RADS category 3 and 4 observations: improved categorization to indicate the risk of hepatic malignancy. AJR Am J Roentgenol. 2020;215:1354-1362.
5. Smereka P, Doshi AM, Lavelle LP, et al. New arterial phase enhancing nodules on MRI of cirrhotic liver: risk of progression to hepatocellular carcinoma and implications for LI-RADS classification. AJR Am J Roentgenol. 2020;215:382-389.
6. Cannella R, Vernuccio F, Celsa C, et al. Long-term evolution of LI-RADS observations in HCV-related cirrhosis treated with directacting antivirals. Liver Int. 2021;41:2179-2188.
7. Ranathunga D, Osman H, Islam N, et al. Progression rates of LR-2 and LR-3 observations on MRI to higher LI-RADS categories in patients at high risk of hepatocellular carcinoma: a retrospective study. AJR Am J Roentgenol. 2022;218:462-470.
8. Kim BJ, Choi SH, Kim SY, et al. Liver Imaging Reporting and Data System categories: Long-term imaging outcomes in a prospective surveillance cohort. Liver Int. 2022;42(7):1648-1657.
Figures