0749
Feasibility of MR phase-contrast imaging for proton beam visualisation in liquid water phantoms1OncoRay – National Center for Radiation Research in Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Helmholtz-Zentrum Dresden-Rossendorf, Dresden, Germany, 2Helmholtz-Zentrum Dresden-Rossendorf, Institute of Radiooncology – OncoRay, Dresden, Germany, 3Technische Universität Dresden, Dresden, Germany, 4Department of Radiotherapy and Radiation Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
Synopsis
Keywords: New Devices, Radiotherapy, Proton Therapy
Proton beam-induced convection in water triggered local MRI magnitude signal loss in combined imaging and irradiation experiments performed on a new research prototype in-beam low-field MRI proton radiotherapy device. In this study, the influence of convection on the MRI phase signal was tested. Both mechanical and thermal inhibition of convection in dedicated water phantoms resulted in the absence of MRI phase signatures, which were clearly visible under conditions were convection could develop. Moreover, a change in either convection velocity or Venc sequence motion sensitivity changed the observed phase contrast, confirming the convection-driven phase contrast mechanism.Introduction
In-beam magnetic resonance imaging (MRI) allows the real-time monitoring of soft tissue motion and is therefore expected to improve the targeting accuracy of proton therapy (PT), particularly for moving tumours¹. Moreover, it has been hypothesised to enable the verification of dose delivery by means of MRI-based proton beam visualisation. With the availability of a first hybrid system integrating low-field MRI and PT², the direct visualisation of the proton beam has proven feasible in liquid-filled phantoms³. The beam-induced signatures observed with MRI were subsequently shown to be triggered by convection resulting in local MRI magnitude signal loss in Time-of-Flight (ToF) angiography images4,5. A possible influence of the beam-induced convection on the MRI phase signal has not been studied to date, but promises velocity encoding gradient-tuneable sensitivity to dose deposition. The aim of the present study was therefore to experimentally assess the feasibility of MR phase-contrast imaging for proton beam visualisation in water phantoms and to test the convection hypothesis for beam-induced phase contrast.Methods
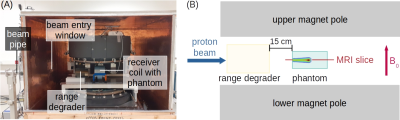
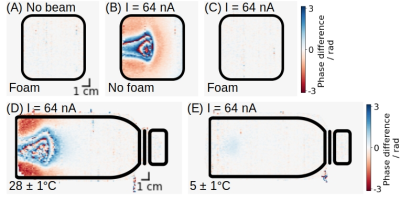
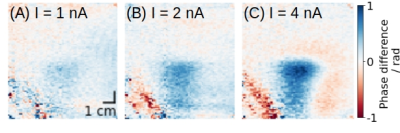
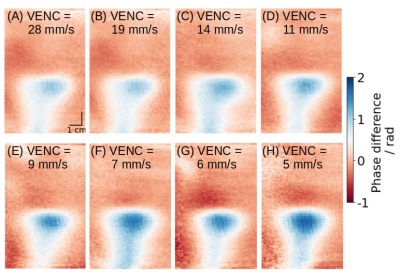
A 0.22 T open MRI scanner (MrJ2200, ASG Superconductors S.p.A., Genoa, Italy) was placed in the beam path of a horizontal proton research beamline2 (Fig. 1A). In simultaneous irradiation and imaging experiments, a 207 MeV proton pencil beam first traversed a range degrader before it was stopped and imaged within water-filled phantoms positioned at the MRI isocentre (Fig. 1B). The feasibility of MRI phase-based proton beam visualisation was assessed during a 32 nA beam current irradiation of a cuboid free-floating water-filled phantom at ambient temperature. The presumed convection origin of the phase signatures was tested under 64 nA current irradiation through the inhibition of convection using either the mechanical restriction of fluid motion in a cuboid foam-filled water phantom at ambient temperature6 or exploiting the temperature dependence of the volumetric expansion coefficient of water to suppress the development of convection in a cylindrical water phantom cooled down to approximately 4 °C7. Each 20 s irradiation was started 15 s prior to image acquisition with a flow-compensated ToF angiography pulse sequence (TE = 7 ms, TR = 19.2 ms, flip angle = 60°, total scan duration = 3 - 4 s). Furthermore, the effect of the variation of either the beam-induced velocities of water convection or the phase sensitivity of the sequence to cross-plane motion was tested using a Velocity Encoding (Venc) pulse sequence (TE = 32 ms, TR = 160 ms, flip angle = 90°, total scan duration = 30 s). While the motion sensitivity parameter VENC was kept fixed at 5 mm/s, the beam current of successive irradiations was increased from 1 to 4 nA, thereby increasing the induced velocities. Moreover, a series of Venc images with VENC ranging from 28 to 5 mm/s were acquired under simultaneous irradiation at 8 nA. The irradiation was started 10 s prior to Venc imaging and terminated at mid-Cartesian acquisition. All single-slice phase-difference images of data acquired with and without simultaneous irradiation were calculated using the complex conjugate method8 and crossed the beam volume horizontally.Results
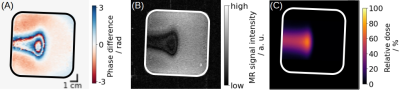
The MRI phase signal showed a clear proton beam-induced signature (Fig. 2A), which was similar in shape and position to both the beam-induced MRI magnitude signature (Fig. 2B) and the pencil beam depth-dose distribution (Fig. 2C) acquired by radiochromic film dosimetry. In contrast to irradiation of free-floating water at ambient temperature (Fig. 3B), the uniform mechanical restriction of water mobility in the foam-filled phantom resulted in an absence of a beam-induced phase shift (Fig. 3C). In contrast to irradiation of free-floating water at an ambient temperature of 28 ± 1 °C (Fig. 3D), irradiation at 5 ± 1 °C also resulted in an absence of a beam-induced phase signature (Fig. 3E). An increase in the beam current setting concomitant with an increase in beam-induced convection velocity resulted in increased phase shifts in Venc images with fixed motion sensitivity (Fig. 4). Furthermore, the Venc phase contrast induced by irradiation at 8 nA beam current was increasable by decreasing VENC (Fig. 5).Discussion
MR phase-contrast imaging for proton beam visualisation has proven feasible using a ToF angiography pulse sequence. Beam-induced phase and magnitude signatures provided comparable geometric information on proton dose deposition. Moreover, similar to the previously assessed MRI magnitude-based beam visualisation5, the induction of a local phase shift relies on convection as demonstrated by the absence of beam-induced phase signatures under mechanical or thermal inhibition of convection. The phase contrast was tuneable by either increasing the beam current concomitant with an increase in convection velocity or by decreasing VENC, thereby increasing the sensitivity of the Venc pulse sequence to cross-plane motion. In combination, these observations confirm the convection hypothesis for phase contrast in that the observed beam-induced phase shifts are evoked by upwards-directed fluid motion.Conclusion
Our experimental results reveal that MR phase-contrast imaging for proton beam visualisation is feasible and that the observed phase signatures are induced by upwards-directed beam-induced convective fluid motion. This method holds potential for application in geometric quality assurance of hybrid MR-integrated PT systems, but requires further enhancement of the sensitivity of Venc imaging to enable beam visualisation at clinically relevant dose levelsAcknowledgements
We thank Andrea Serra and Marco Battiston from ASG Superconductors S.p.A. (Genoa, Italy) for their support and the fruitful discussions.References
1 Hoffmann A, Oborn B, Moteabbed M, et al. MR-guided proton therapy: a review and a preview. Radiat Oncol. 2020;15:1-13.
2 Schellhammer S, Hoffmann A, Gantz S, et al. Integrating a low-field open MR scanner with a static proton research beam line: proof of concept. Phys Med Biol. 2018;63(23):23LT01.
3 Schellhammer S. Technical feasibility of MR-integrated proton therapy: beam deflection and image quality. Doctoral thesis. Technische Universität Dresden. 2019. https://nbn- resolving.org/urn:nbn:de:bsz:14-qucosa2-341326. Accessed October 11, 2022.
4 Gantz S. Feasibility of in-beam MR imaging for actively scanned proton beam therapy. Doctoral thesis. Technische Universität Dresden. 2022. https://nbn-resolving.org/urn:nbn:de:bsz:14-qucosa2-794329. Accessed October 11, 2022.
5 Peter J, Gantz S, Karsch L, et al. Convection triggers local MR signal loss during proton beam irradiation of liquid water phantoms. Proc. Intl. Soc. Mag. Reson. Med. 30.2022;2732.
6 Domen S, Krauss A and Roos M. The problem of convection in the water absorbed dose calorimeter. Thermochim acta. 1991;187:225-233.
7 Schulz R and Weinhous M. Convection currents in a water calorimeter. Phys Med Biol. 1985;30(10):1093-1099.
8 Price R, Allison J, Clarke G et al. for the American College of Radiology Committee on Quality Assurance in Magnetic Resonance Imaging. 2015 Magnetic Resonance Imaging Quality Control Manual. ACR 2015;72-86.
Figures