0732
Evaluating intra-voxel incoherent motion in the uterine cervix: healthy volunteer repeatability and therapy-induced changes in tumours1Division of Cancer Sciences, The University of Manchester, Manchester, United Kingdom, 2Clinical Radiology, The Christie NHS Foundation Trust, Manchester, United Kingdom, 3Christie Medical Physics and Engineering, The Christie NHS Foundation Trust, Manchester, United Kingdom, 4School of Medicine, University of Leeds, Leeds, United Kingdom, 5Clinical Oncology, The Christie NHS Foundation Trust, Manchester, United Kingdom, 6Clinical Oncology, Mount Vernon Cancer Centre, Northwood, United Kingdom, 7Division of Radiotherapy and Imaging, Institute of Cancer Research, London, London, United Kingdom
Synopsis
Keywords: Uterus, Cancer
There is a need for robust imaging biomarkers which can be used to assess early tumour response to therapy. Intra-voxel incoherent motion (IVIM) can provide information about tumour microstructure and microvasculature, but requires technical and biological validation. This work evaluates IVIM repeatability in the uterine cervix of healthy volunteers, assesses the sensitivity of IVIM parameters to therapy in patients with uterine cervical cancer, and evaluates model suitability through a model comparison framework.Introduction
Functional MRI provides quantitative imaging biomarkers that can be used to evaluate tumour response to therapy. Intra-voxel incoherent motion (IVIM) can provide information about tumour microstructure and microvasculature, but the IVIM model may not be applicable in all tumour regions 1. This work uses a model comparison framework to assess the spatial variability in the IVIM model’s suitability, in healthy uterine cervix tissue and in cervical tumours. The repeatability of IVIM parameters is evaluated through repeat scans of healthy volunteers, and the sensitivity of IVIM parameters to therapy-induced changes is assessed in patients. This work contributes to the technical and biological validation 2 of biomarkers from diffusion-weighted MRI.Methods
AcquisitionImaging was performed on a 1.5 T Philips Ingenia MR-RT, following ethics approval (REC: 20/NW/0377)3. Six healthy volunteers (age: 26±1.3) were scanned twice, 19±25 days apart (range: 7-70). Eight patients (age: 47±17.5) with locally advanced (stages IIB-IVA) squamous cell carcinoma were scanned at three timepoints: pre-treatment, week 3, and week 5 of treatment. All patients underwent standard of care treatment: weekly cisplatin chemotherapy prescribed at 40 mg/m2; combined chemoradiation/brachytherapy prescribed to reach a final dose of 85-90 Gy EQD2. The same multiparametric MR protocol was used for patients and healthy volunteers, including a sagittal PGSE-EPI diffusion acquisition with b = 0, 20, 40, 60, 80, 100, 150, 300, 500, 800 s/mm2, TR = 2800 ms, TE = 61 ms, voxel size = 2.9 x 2.9 x 6.0 mm3.
Analysis
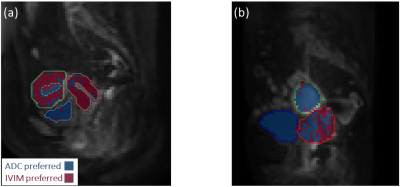
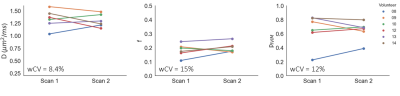
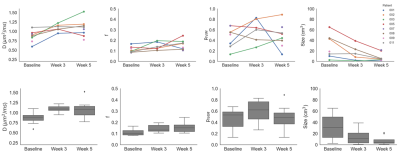
Initial processing was performed using the Madym toolkit 4. IVIM and apparent diffusion coefficient (ADC) models were fitted voxel-wise to data at all b-values, and the fits were statistically compared using the corrected Akaike information criterion (AICc), which is used when the number of data points is small relative to the number of estimated parameters. IVIM parameter maps (diffusion coefficient, D, and perfusion signal fraction, f) were generated, along with model preference maps showing which model was favoured in each voxel. ADC-favoured voxels are expected to reflect regions with a single tissue diffusion component, while IVIM-favoured voxels are expected to reflect well-perfused regions. Uterine cervix regions of interest (ROIs) were defined for healthy volunteers, and whole-tumour ROIs were defined for patients. Median IVIM parameter values were obtained, along with the fraction of voxels in which the IVIM model was favoured, termed pIVIM. Repeatability was quantified using the within-subject coefficient of variation (wCV) for the healthy volunteer data. Differences in parameters between healthy cervix tissue and cervical tumours were evaluated with unpaired t-tests, comparing the mean of the repeated measurements from healthy volunteers with the pre-treatment measurements from patients. The sensitivity of IVIM parameters to early therapy-induced changes was evaluated using paired t-tests, comparing pre-treatment and week 3 values from the six patients who had both of these scans.
Results
Example model preference maps are shown in Figure 1 for a healthy volunteer and patient. ADC can be seen to be favoured in the bladder and uterine cavity fluid, while IVIM was preferred in the uterine myometrium and cervix; in healthy volunteer cervical tissue pIVIM = 0.65 ± 0.17 (mean ± SD across all subjects and repeat scans). In the tumour, there is spatial variation in the preferred model. Healthy volunteer repeatability is shown in Figure 2, plotting median D, median f, and pIVIM, which have wCV = 8.4%, 15%, and 12%, respectively. Parameter values in healthy cervix tissue and cervical tumours are compared in Figure 3, showing significantly lower D (p < 0.0001) and lower f (p < 0.001) in tumours. There is a trend towards lower pIVIM in tumours, but this is not significant (p = 0.096). Median D, median f, and pIVIM for all tumours and timepoints are shown in Figure 4. D significantly increased from baseline to week 3 (p = 0.015), while f showed no significant change (p = 0.099). The fraction of tumour voxels favouring IVIM showed large inter-patient variability (range at baseline: 0.13 – 0.68), which was maintained throughout treatment. Reliable contouring was hampered for some tumours at week 5 due to their small size.Discussion
The model preference maps reflect expected trends based on tissue characteristics, with ADC tending to be preferred in non-vascularised regions, and IVIM tending to be favoured in vascular tissue. While this contributes to the validation of the model comparison framework, it should be noted that the accuracy of model comparison approaches has been shown to decrease with lower signal-to-noise ratios5, which may lead to an underestimation of pIVIM. All parameters exhibit good repeatability in the cervix of healthy volunteers, with D being the most repeatable. Some of the variability in diffusion and perfusion characteristics may stem from the repeated scans being performed at different times in the subjects’ menstrual cycle, with variations in ADC previously observed across the menstrual phases6. D and f differ significantly between healthy volunteers and patients, consistent with previous reports comparing cervical tumours with healthy cervix tissue7. D is the only parameter showing early sensitivity to treatment-induced changes, with an increase in D consistent with previous reports of ADC increases following therapy8.Acknowledgements
This work was supported by the Cancer Research UK Manchester Centre award [CTRQQR-2021\100010] and the NIHR Manchester Biomedical Research Centre.References
1. Winfield JM, Orton MR, Collins DJ, et al. Separation of type and grade in cervical tumours using non-mono-exponential models of diffusion-weighted MRI. Eur Radiol. 2017 Feb;27(2):627-636. doi: 10.1007/s00330-016-4417-0. Epub 2016 May 24. PMID: 27221560; PMCID: PMC5209433.
2. O'Connor JP, Aboagye EO, Adams JE, et al. Imaging biomarker roadmap for cancer studies. Nat Rev Clin Oncol. 2017 Mar;14(3):169-186. doi: 10.1038/nrclinonc.2016.162. Epub 2016 Oct 11. PMID: 27725679; PMCID: PMC5378302.
3. Datta et al., ISMRM 2022; 2584.
4. Berks M, Parker G, Little R, Cheung S. Madym: A C++ toolkit for quantitative DCE-MRI analysis. Journal of Open Source Software. 2021 Oct 7;6(66).
5. McHugh DJ, Lipowska-Bhalla G, Babur M, et al. Diffusion model comparison identifies distinct tumor sub-regions and tracks treatment response. Magn Reson Med. 2020 Sep;84(3):1250-1263. doi: 10.1002/mrm.28196. Epub 2020 Feb 14. PMID: 32057115; PMCID: PMC7317874.
6. Fang et al., ISMRM 2022; 0916.
7. Lee EY, Yu X, Chu MM, et al. Perfusion and diffusion characteristics of cervical cancer based on intraxovel incoherent motion MR imaging-a pilot study. Eur Radiol. 2014 Jul;24(7):1506-13. doi: 10.1007/s00330-014-3160-7. Epub 2014 Apr 19. PMID: 24744198.
8. Fu ZZ, Peng Y, Cao LY, et al. Value of apparent diffusion coefficient (ADC) in assessing radiotherapy and chemotherapy success in cervical cancer. Magn Reson Imaging. 2015 Jun;33(5):516-24. doi: 10.1016/j.mri.2015.02.002. Epub 2015 Feb 7. PMID: 25660642.
Figures