0731
Value of multiple mathematical models of advanced zoomed DWI for the evaluation of tumor-stroma ratio in rectal cancer1National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 2Beijing No.4 High School International Campus, Beijing, China, 3MR Scientific Marketing, Siemens Healthineers Ltd., Beijing, China, 4Shanghai Key Laboratory of Magnetic Resonance, East China Normal University, Shanghai, China
Synopsis
Keywords: Pelvis, Cancer, Tumor microenvironment
Tumor-stroma ratio (TSR) can reflect the relationship between tumor cells and tumor microenvironment. Evaluation of the TSR timely and accurately is important because of its role in predicting prognosis and making individualized treatment plans. Diffusion parameters obtained from multiple mathematical models of DWI can reflect microscopic characteristics of tumors. Multi b-value DWI with the advanced zoomed DWI technology can provide a higher-spatial-resolution with less artifacts. This study aimed to investigate the value of zoomed multi b-value DWI for predicting TSR in rectal cancer. The results suggested that distributed diffusion coefficient (DDC) is a promising indicator to identify high TSR group.Introduction
Tumor-stroma ratio (TSR), which indicates the proportions of stroma area relative to tumor tissue, has been proven to be a strong prognostic factor for patients with rectal cancer1,2. However, it is difficult to accurately determine the TSR score before surgery. With the development of diffusion techniques, diffusion models (i.e. mono-, bi-, and stretched exponential models) have shown high diagnostic performance in assessing tumor grade, treatment response, and prognosis3-5. The purpose of this study was to investigate the utility of diffusion parameters that derived from advanced zoomed multi b-value DWI in preoperative evaluation of TSR in patients with rectal cancer.Methods
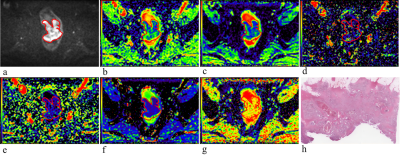
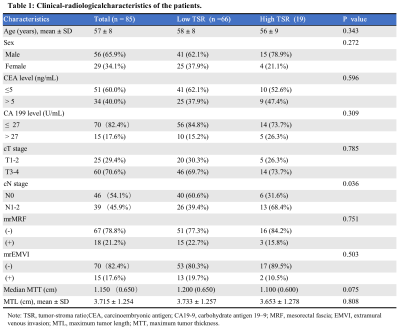
From July 2020 and July 2021, a total of 85 patients (mean age ± standard deviation, 57 ± 8 years; 56 males) with histopathological confirmed rectal adenocarcinoma were prospectively enrolled. All patients underwent MRI examination including the advanced zoomed DWI sequence (prototypic non-parallel transmission zoomed EPI DWI sequence) with b-values of 0, 20, 40, 80, 160, 200, 400, 800, 1200, and 1600s/mm2 on a 3T MRI scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany). The apparent diffusion coefficient (ADC) from the mono-exponential model, the true diffusion coefficient (D), pseudo-diffusion coefficient (D*), and perfusion fraction (f) from the bi-exponential model, and the distributed diffusion coefficient (DDC) and the water molecular diffusion heterogeneity index (α) from the stretched exponential model were calculated. Intraclass correlation coefficient (ICC) was used to quantify the interobserver agreement. For both clinical-radiological characteristics and diffusion parameters, univariable and multivariable analysis were used to evaluate associations with the TSR. The diagnostic performance was assessed using area under the receiver operating characteristic curve (AUC) and compared with the Delong method.Results
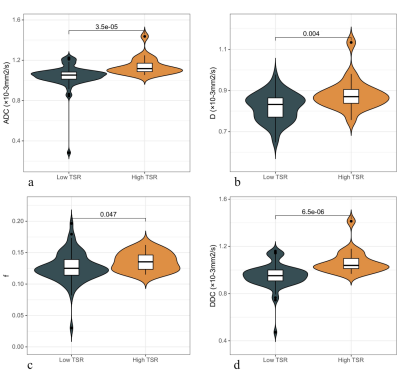
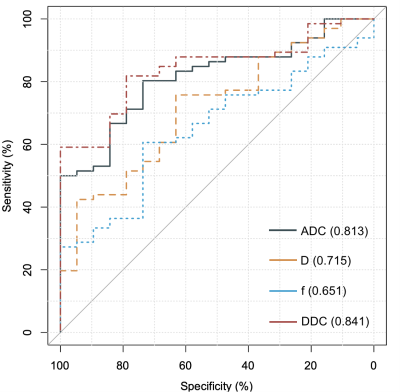
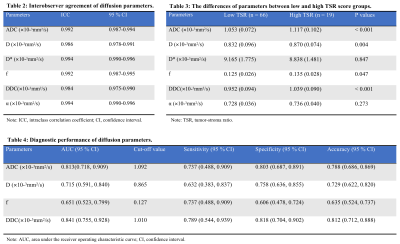
Of the 85 patients, 66 (77.6%) had low TSR score (≤ 50%) and 19 (22.4%) had high TSR score (> 50%). ICCs were excellent for all diffusion parameters, with the range of 0.984-0.994. High TSR rectal tumors showed significantly higher ADC (median 1.117 vs 1.053 ×10-3mm2/s, p < 0.001), D (median 0.870 vs 0.832 ×10-3mm2/s, p = 0.004), f (median 0.135 vs 0.125, p = 0.046), and DDC (median 1.039 vs 0.952 ×10-3mm2/s, p < 0.001) values than low TSR tumors. The AUCs of ADC, D, f, and DDC were 0.813 (95% confidence interval [CI], 0.718-0.909), 0.715 (95% CI, 0.591-0.840),0.651 (95% CI, 0.523-0.799), and 0.841 (95% CI, 0.755-0.928), respectively. According to multivariable analysis, DDC was independently correlated with TSR of rectal cancer (odds ratio = 1.013; 95% CI: 1.006-1.021). The diagnostic performance of DDC was better than that of the clinical-radiological model (AUC, 0.645 [95% CI, 0.522-0.768]; p = 0.008).Discussion
In rectal cancer, patients with high TSR tend to have a worse overall and disease-free survival than do patients with low TSR1,2. However, TSR is traditionally obtained by histopathologic evaluation after surgery, which limits its clinical application. Multi b-value DWI using multiple mathematical models could provide physiological and molecular information of the in-vivo tumor tissue. Bi-exponential model could allow separate estimation of microcirculation in the capillaries and molecular diffusion; it has been widely used in assessing tumor grade, treatment response, and prognosis3-5. The stretched exponential model focuses on spatial heterogeneity of diffusion within voxels, which could be a potential biomarker for changes of tissue complexity and microenvironment. However, multi b-value DWI using conventional ss-EPI DWI technology has many limitations, such as limited spatial resolution, sensitivity to motion and magnetic field inhomogeneity, and susceptibility artifacts from gas in rectum which may cause image distortion. The advanced zoomed DWI (prototypic non-parallel transmission zoomed EPI DWI) applies a 2D excitation RF pulse with tilted field of excitation6,7. It selectively excites the selected field-of-view to decrease artifacts and distortion, while tilting the excitation plane avoids that unwanted side excitation lead to in-folding artifacts. Therefore, multi b-value DWI using the advanced zoomed DWI technology makes it possible to obtain more detailed information of the rectal tumor. This current study evaluated the feasibility of using advanced zoomed multi b-value DWI for the preoperative assessment of TSR in patients with rectal cancer. The results demonstrated that ADC, D, f, and DDC values, which were obtained from multiple models of advanced zoomed EPI DWI, have potential to differentiate high TSR from low TSR rectal cancers. DDC from the stretched exponential model achieved the highest AUC among all diffusion parameters, and was superior to the clinical-radiological model.Conclusion
DDC from the stretched exponential model showed excellent predictive performance, and multi b-value DWI with the advanced zoomed DWI technology may be a non-invasive and useful tool for identifying patients with high TSR score in rectal cancer.Acknowledgements
The authors acknowledge Thomas Benkert for his assistance with technical support of the advanced zoomed DWI sequence.References
1. Yang L, Chen P, Zhang L, et al. Prognostic value of nucleotyping, DNA ploidy and stroma in high-risk stage II colon cancer. Br J Cancer. 2020 Sep;123(6):973-981.
2. Zhao Z, Zhang X, Li Z, et al. Automated assessment of DNA ploidy, chromatin organization, and stroma fraction to predict prognosis and adjuvant therapy response in patients with stage II colorectal carcinoma. Am J Cancer Res. 2021 Dec 15;11(12):6119-6132.
3. Almutlaq ZM, Wilson DJ, Bacon SE, et al. Evaluation of Monoexponential, Stretched-Exponential and Intravoxel Incoherent Motion MRI Diffusion Models in Early Response Monitoring to Neoadjuvant Chemotherapy in Patients With Breast Cancer-A Preliminary Study. J Magn Reson Imaging. 2022 Oct;56(4):1079-1088.
4. Zhao L, Liang M, Yang Y, et al. Histogram models based on intravoxel incoherent motion diffusion-weighted imaging to predict nodal staging of rectal cancer. Eur J Radiol. 2021 Sep;142:109869.
5. Liang CY, Chen MD, Zhao XX, et al. Multiple mathematical models of diffusion-weighted magnetic resonance imaging combined with prognostic factors for assessing the response to neoadjuvant chemotherapy and radiation therapy in locally advanced rectal cancer. Eur J Radiol. 2019 Jan;110:249-255.
6. Finsterbusch J. Improving the performance of diffusion-weighted inner field-of-view echo-planar imaging based on 2D-selective radiofrequency excitations by tilting the excitation plane. J Magn Reson Imaging. 2012 Apr;35(4):984-92.
7. Hu L, Zhou DW, Fu CX, et al. Advanced zoomed diffusion-weighted imaging vs. full-field-of-view diffusion-weighted imaging in prostate cancer detection: a radiomic features study. Eur Radiol. 2021 Mar;31(3):1760-1769.
Figures