0728
Combined IVIM and DKI MRI in pre-operative assessment of bladder cancer with different stages and grades1Qilu Hospital of Shandong University, Jinan, China, 2GE Healthcare, MR Research China, Beijing, China
Synopsis
Keywords: Urogenital, Bladder
This study aimed to determine the feasibility of intravoxel-incoherent-motion(IVIM) and diffusion-kurtosis-imaging (DKI) parameters in differentiating tumor stages and grades of bladder cancers preoperatively. The IVIM-related parameter (true-diffusion-coefficient) and DKI-related parameters (mean-diffusivity; mean-kurtosis) were significantly higher in non–muscle-invasive than muscle-invasive bladder cancers, and in low-grade than high-grade ones (all p <0.05). Robust diagnostic efficacies were separately confirmed with high AUCs for IVIM and DKI in staging and grading bladder cancers, and the optimal efficacy was obtained with combined IVIM and DKI models. Therefore, combined IVIM and DKI might be considered effective in differentiating the stages and grades of bladder cancers.
INTRODUCTION
The tumor stage and grade of bladder cancer are primarily associated with its clinical treatment and prognosis.[1] Therefore, it is thus essential to accurately diagnose tumor stage and histological grade of bladder cancer in the clinic.Intravoxel-incoherent-motion diffusion-weighted-imaging (IVIM-DWI) can reflect both perfusion and diffusion-related effects in tumors, thus accurately characterizing the molecule diffusion pattern of tumors without contrast agent injection.[2] Meanwhile, diffusion kurtosis imaging (DKI), developed based on an advanced diffusion model, is able to provide additional information regarding the deviation of water diffusion away from Gaussian distribution, which is related to the irregularity and heterogeneity of cellular microstructures.[3] Several previous studies have separately used IVIM or DKI in evaluating the diagnostic values in grading and staging bladder cancers.[4,5] Although good results were obtained, distinctive physiological and pathological features of bladder cancer, including tumor cellularity, heterogeneity, and perfusion, cannot be comprehensively evaluated with either single technique. The combination of both techniques might hold more clinical potential in differentiating bladder cancers but has not been studied so far.
Therefore, the purpose of this study was to investigate if combined diffusion parameters from IVIM and DKI models were feasible in grading and staging bladder cancers.
METHODS
Subjects42 patients (median age, 65 years; range, 21-80 years) known or suspected to have bladder cancers were recruited in this study. Certain exclusion criteria were defined as follows: (1) chemotherapy performed before MRI examination (2) lesion smaller than 5 mm (3) patient motion or inadequate image quality.
MRI acquisition
All MR experiments were performed at a 3.0T-MR system (Discovery 750w, GE Healthcare, USA) with a 16-channel coil employed. IVIM and DKI imaging were performed on the bladder after acquiring the corresponding T2-weighted anatomical images.
For IVIM, a single shot spin-echo echo-planar imaging sequence was applied in axial view with 11 b-values (0, 10, 25, 50, 75, 100, 150, 200, 400, 800, and 1000s/mm2). TR/TE,4000/80.4ms; field-of-view, 32cm×32cm; matrix, 128×128; slice thickness, 4mm; scan time, 2mins 46s.
For DKI, a separate single-shot spin-echo echo-planar imaging sequence with 6 b-values (0, 400, 800, 1200, 1600, and 2000s/mm2) with 15 diffusion directions per b value was applied. Other scan parameters were TR/TE,6000/126ms; field-of-view, 32cm×32cm; matrix, 128×128; slice thickness, 4mm; scan time, 7mins 43s.
Data analysis
IVIM and DKI data were separately analyzed using IVIM and DKI post-processing software developed in the GE ADW4.6 workstation. The IVIM related parameters including true diffusion coefficient (D), perfusion related pseudo-diffusion coefficient (D*) and perfusion fraction (f), and DKI parameters of mean diffusivity (MD) and mean kurtosis (MK), were obtained accordingly.
Two senior radiologists were employed to place regions of interest (ROI)s on the slice showing the largest cross-section section of the tumor that was greater than 5mm. All parameter values of ROIs were measured three times and the corresponding mean values were obtained for further data analysis.
SPSS 22.0 statistic software was used for statistic analyses. Intra-class correlation coefficients analysis (ICC) was applied to assess the inter-observer agreement of parameter measurements over two radiologists. The Mann-Whitney U test was used for comparing each parameter between high-grade and low-grade, and between non–muscle-invasive and muscle-invasive bladder cancers. Receiver operating characteristic (ROC) analyses were further performed to separately evaluate the diagnostic performances of IVIM and DKI parameters with significant differences, and the combined model with these parameters was included. The significance threshold was set as P<0.05.
RESULTS
In total 12 low-grade and 18 high-grade patients, and 17 non–muscle-invasive and 13 muscle-invasive patients were included for data analysis.Excellent inter-observer agreements of diffusion parameter measurements were confirmed by high ICCs, ranging between 0.879 and 0.956.
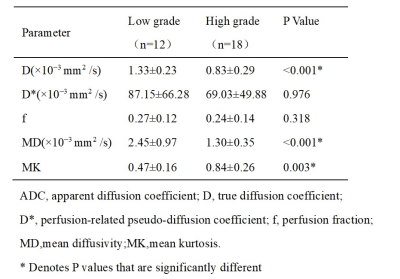
D and MD were significantly higher in the non-muscle-invasive than muscle-invasive bladder cancers (1.18±0.27×10−3mm2/s vs 0.82±0.33×10−3mm2/s, 2.03±0.89×10−3mm2/s vs 1.35±0.69×10−3mm2/s; P<0.05)(Tab.1, Fig.1) and in low-grade than high-grade ones (1.33±0.23×10−3mm2 /s vs 0.83±0.29×10−3mm2/s,2.45±0.97×10−3mm2/s vs 1.30±0.35×10−3mm2/s; P<0.05)(Tab.2, Fig.2). For MK, an opposite pattern was found between non–muscle-invasive and muscle-invasive bladder cancers (0.57±0.25vs0.90±0.21, P<0.05) and between low-grade bladder than high-grade bladder cancers (0.47±0.16vs0.84±0.26, P<0.05). Comparable D* and f values were observed between each two groups (P>0.05).
The areas under the ROC curve of D, MD, and MK were 0.838, 0.850, and 0.829 in staging bladder cancers(Fig.3a); and 0.911, 0.875, and 0.933 in grading bladder cancers, respectively(Fig.3b). The AUCs of the combined D, MD and MK were improved to 0.949 in staging and 0.938 in grading bladder cancers.
DISCUSSION
Our results demonstrated that the diffusion parameters (D, MD, MK) were significantly different in bladder cancers with various stages and grades. This may partly be explained by their histopathological characteristics. As the pathological grade and stage increased, the number of tumor cells increased, tissue disturbance increased and extracellular space curvature decreased, contributing to the altered diffusion behaviors of water molecules.CONCLUSION
In conclusion, combined IVIM and DKI related parameters may be effective imaging biomarkers for predicting bladder cancer stage and grade.Acknowledgements
No acknowledgement found.
References
1. Josephson D, Pasin E, Stein JP. Superficial bladder cancer: part 2. Management. Expert Rev Anticancer Ther. 2007;7(4):567-581.
2. Bennett KM, Schmainda KM, Bennett RT, et al. Characterization of continuously distributed cortical water diffusion rates with a stretched-exponential model. Magn Reson Med. 2003;50(4):727-734.
3. Jensen JH, Helpern JA. MRI quantification of non-Gaussian water diffusion by kurtosis analysis. NMR Biomed. 2010;23(7):698-710.
4. Wang Y, Hu D, Yu H, et al. Comparison of the Diagnostic Value of Monoexponential, Biexponential, and Stretched Exponential Diffusion-weighted MRI in Differentiating Tumor Stage and Histological Grade of Bladder Cancer. Acad Radiol. 2019;26(2):239-246.
5. Li Q, Cao B, Tan Q, et al. Prediction of muscle invasion of bladder cancer: A comparison between DKI and conventional DWI. Eur J Radiol. 2021;136:109522.
Figures
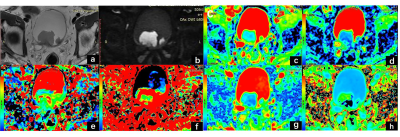
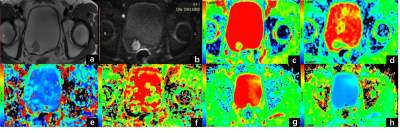
Figure 2 A 65-year-old man with pathologically confirmed low-grade no muscle invasive bladder cancer . The lesion showed high signal intensity (SI) on T2- weighted image (a) and diffusion image(b). (c-h) Corresponding parametric maps (ADC, D, D*,f, MD, MK). Tumor values were 1.68×10 -3mm2 /s, 1.26×10-3 mm2 /s, 13.8×10-3 mm2 /s, 1.99, 0.69, 0.33, respectively.
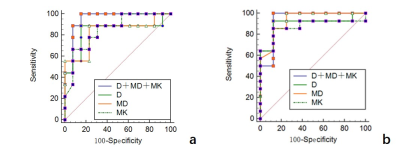
Figure 3.
a. Receiver operating characteristic curves for D,MD and MK, and the combination of D, MD and MK in differentiating non-muscle-invasive from muscle-invasive bladder cancers.
b. Receiver operating characteristic curves for D, MD, and MK, and the combination of D, MD, and MK in differentiating low-grade from high-grade bladder cancers.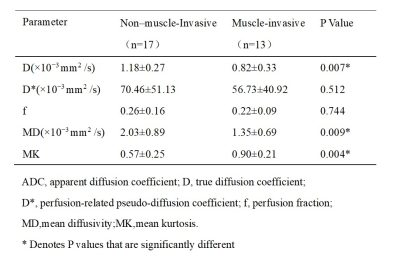
Table 1. Comparisons of IVIM and DKI -related parameter values between non–muscle-invasive bladder cancers and muscle-invasive cancers