0726
Detection rate of prostate cancer using mpMRI-Inbore targeted prostate biopsy, mpMRI-TRUS guided biopsy and TRUS guided biopsy
Sujeet Kumar Mewar1, Sanjay Sharma2, Ekta Dhamijia3, Sanjay Thulkar3, S. Datta Gupta4, Sridhar Panaiyadiyan5, Naranamangalam R. Jagannathan6, Rajeev Kumar5, and Virendra Kumar 1
1Department of N.M.R., All India Institute of Medical Sciences, New Delhi, India, 2Department of Radio-diagnosis , RPC, All India Institute of Medical Sciences, New Delhi, India, 3Department of Radio-diagnosis, IRCH, All India Institute of Medical Sciences, New Delhi, India, 4Department of Pathology, All India Institute of Medical Sciences, New Delhi, India, 5Department of Urology, All India Institute of Medical Sciences, New Delhi, India, 6Department of Radiology, Present address. Chettinad Academy of Research and Education, Kelambakkam., Tamil Nadu, India
1Department of N.M.R., All India Institute of Medical Sciences, New Delhi, India, 2Department of Radio-diagnosis , RPC, All India Institute of Medical Sciences, New Delhi, India, 3Department of Radio-diagnosis, IRCH, All India Institute of Medical Sciences, New Delhi, India, 4Department of Pathology, All India Institute of Medical Sciences, New Delhi, India, 5Department of Urology, All India Institute of Medical Sciences, New Delhi, India, 6Department of Radiology, Present address. Chettinad Academy of Research and Education, Kelambakkam., Tamil Nadu, India
Synopsis
Keywords: Prostate, MR-Guided Interventions
The present study demonstrated the comparison of detection rate of PCa between the three groups of patients recruited based on PSA > 4 ng/ml and abnormal DRE. The PCa detection rate of mpMRI-Inbore biopsy (Group I) was found 50 % while for mpMRI-TRUS guided biopsy (Group II) 26 %. The combined detection rate of techniques with and without mpMRI was also calculated and found 44 %, for mpMRI-Inbore biopsy and mpMRI-TRUS guided biopsy, while 34.5 %, in TRUS guided biopsy (Group III). Study shows that there is a significant advantage of mpMRI Inbore biopsy compared to TRUS guided prostate biopsy.Introduction:
Prostate cancer (PCa) is the second most common cancer among men over the age of 50 years. Serum prostate specific antigen (PSA) level and a digital rectal examination (DRE) are used as screening test and prostate biopsy is the diagnostic test. Using mpMRI before the biopsy, can improve the detection and staging of cancer, location of lesions, and evaluation of aggressiveness of cancer. Here the aim of our study is to evaluate the detection rate of clinically significant PCa, based on PIRADS version 2.1 scoring. Study represents the comparison of detection rate of PCa between mpMRI-Inbore prostate biopsy, mpMRI-TRUS guided biopsy and TRUS guided prostate biopsy1.
Methods:
Patients were recruited based on PSA > 4 ng/ml and abnormal DRE. MRI investigations were carried out at 3.0 T MRI system (Achieva, Philips, Netherlands). Patients were divided in to three groups: Group I, n = 56 patients, (mean age, 65 ± 6.8 years, median PSA, 12.9 ng/ml) who underwent mpMRI-Inbore biopsy, Group II, n = 19 patients (mean age, 66.52 ± 6.88 years, median PSA 14.30 ng/ml) who underwent mpMRI-TRUS guided biopsy, and Group III, n = 110 patients (mean age, 65 ± 8 years, median PSA 14.9 ng/ml) who underwent only TRUS guided prostate biopsy. mpMRI was done one week prior the biopsy and images were acquired using different sequences like, T1-WI, T2-WI, DWI, and DCE-MRI in mpMRI. T2W images and DWI images were acquired using parameters: repetition time (TR) of 6100 ms, echo time (TE) of 100 ms, field of view = 240 x 240 mm, slice thickness 3 mm, and seven b-values 0, 200, 400, 800, 1000, 1500 and 2000 s/mm2, respectively. Apparent diffusion coefficient (ADC) of tumor regions was calculated from ADC map. For DCE-MRI, 20 ml Gadolinium was injected at a rate of 3ml/s and T1W images were obtained after every 2-5 s. Group I patients underwent mpMRI-Inbore biopsy on the suspicious areas directly, in the bore of the magnet using a DynaTrim (Invivo, USA) biopsy device with needle guide and DynaCad software. Biopsy was carried out by transrectal approach and localization of lesion was confirmed using MR imaging before targeted biopsy. Three to six cores were collected from the suspicious areas. All lesions were assigned a score based on PIRADS classification system. For Group II and Group III patients only mpMRI TRUS biopsy and TRUS guided prostate biopsy was carried out respectively, by transrectal approach. Institute ethics committee approved the study and informed consent was taken from all subjects.
Results:
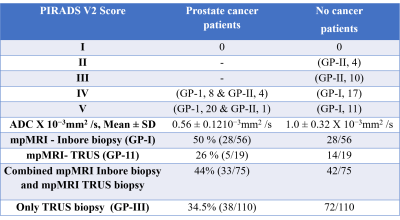
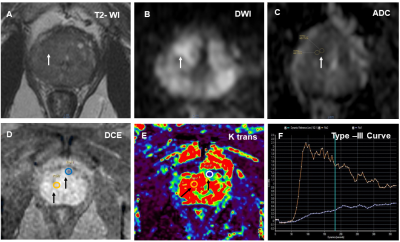
The PCa detection rate between the three groups of patients, namely n = 56 patients (Group I) underwent mpMRI-Inbore biopsy, n = 19 patients (Group II) mpMRI-TRUS guided biopsy and n = 110 patients (Group III) who underwent TRUS guided biopsy were compared. PIRADS scores of targeted lesions of mpMRI were correlated with the histopathological findings. Figure 1 (A-F) shows the result of 53-year-old patient with PSA level (39 ng/ml), mpMRI and MR guided Inbore prostate biopsy with Gleason score 8(4+4) PCa. The mean ADC showed significant difference between patients of PCa (0.56 ± 0.12 X 10−3mm2 /s), and patients with no evidence of cancer (1.0 ± 0.32 X 10−3mm2 /s) (Table 1). The PCa detection rate of mpMRI-Inbore biopsy was found 50 % (28/56) and for clinically significant cancer it was 93 % (26/28) while for mpMRI-TRUS guided biopsy 26 % (5/19). All the 5 patients of mpMRI-TRUS biopsy were found clinically significant cancer. The combined detection rate of techniques with and without mpMRI was also calculated and found 44 % (33/75), for mpMRI-Inbore biopsy and mpMRI-TRUS guided biopsy, for clinically significant cancer 93.9 % (31/33) while 34.5 % (38/110), in TRUS guided prostate biopsy and 73.6 % (28/38) for clinically significant cancer (Table 1). Clinically significant cancer having Gleason score 7 (3+4) or higher were included in study. Our study demonstrated that mpMRI accurately identified suspicious areas of lesion and helped to target these areas with accuracy for diagnosis of clinically significant cancer. The biopsy yields in mpMRI-Inbore biopsy 42.2% (140/331) and in mpMRI-TRUS guided biopsy 16.6% (46/276) while in TRUS guided prostate biopsy 27% (358/1320) were obtained as per the number of cores taken.
Discussion:
Our study demonstrated that, mpMRI-Inbore biopsy has higher detection rate of PCa, compared to mpMRI-TRUS guided biopsy and TRUS guided prostate biopsy2. The overall detection rate of combined mpMRI guided prostate biopsy was higher compared with TRUS guided prostate biopsy. The use of ADC may reduce the number of false positive findings as well as unnecessary biopsies cores. The detection rate using mpMRI was significantly higher in patients having PIRADS scores 4 and 5 than the patients of PIRADS score 3 and 2. Study shows that there is a significant advantage of mpMRI-Inbore biopsy compared to TRUS guided biopsy.
Conclusion:
mpMRI-guided Inbore biopsy showed better detection rate of PCa compared to two groups that is mpMRI-TRUS prostate biopsy and TRUS prostate biopsy.
Prostate cancer (PCa) is the second most common cancer among men over the age of 50 years. Serum prostate specific antigen (PSA) level and a digital rectal examination (DRE) are used as screening test and prostate biopsy is the diagnostic test. Using mpMRI before the biopsy, can improve the detection and staging of cancer, location of lesions, and evaluation of aggressiveness of cancer. Here the aim of our study is to evaluate the detection rate of clinically significant PCa, based on PIRADS version 2.1 scoring. Study represents the comparison of detection rate of PCa between mpMRI-Inbore prostate biopsy, mpMRI-TRUS guided biopsy and TRUS guided prostate biopsy1.
Methods:
Patients were recruited based on PSA > 4 ng/ml and abnormal DRE. MRI investigations were carried out at 3.0 T MRI system (Achieva, Philips, Netherlands). Patients were divided in to three groups: Group I, n = 56 patients, (mean age, 65 ± 6.8 years, median PSA, 12.9 ng/ml) who underwent mpMRI-Inbore biopsy, Group II, n = 19 patients (mean age, 66.52 ± 6.88 years, median PSA 14.30 ng/ml) who underwent mpMRI-TRUS guided biopsy, and Group III, n = 110 patients (mean age, 65 ± 8 years, median PSA 14.9 ng/ml) who underwent only TRUS guided prostate biopsy. mpMRI was done one week prior the biopsy and images were acquired using different sequences like, T1-WI, T2-WI, DWI, and DCE-MRI in mpMRI. T2W images and DWI images were acquired using parameters: repetition time (TR) of 6100 ms, echo time (TE) of 100 ms, field of view = 240 x 240 mm, slice thickness 3 mm, and seven b-values 0, 200, 400, 800, 1000, 1500 and 2000 s/mm2, respectively. Apparent diffusion coefficient (ADC) of tumor regions was calculated from ADC map. For DCE-MRI, 20 ml Gadolinium was injected at a rate of 3ml/s and T1W images were obtained after every 2-5 s. Group I patients underwent mpMRI-Inbore biopsy on the suspicious areas directly, in the bore of the magnet using a DynaTrim (Invivo, USA) biopsy device with needle guide and DynaCad software. Biopsy was carried out by transrectal approach and localization of lesion was confirmed using MR imaging before targeted biopsy. Three to six cores were collected from the suspicious areas. All lesions were assigned a score based on PIRADS classification system. For Group II and Group III patients only mpMRI TRUS biopsy and TRUS guided prostate biopsy was carried out respectively, by transrectal approach. Institute ethics committee approved the study and informed consent was taken from all subjects.
Results:
The PCa detection rate between the three groups of patients, namely n = 56 patients (Group I) underwent mpMRI-Inbore biopsy, n = 19 patients (Group II) mpMRI-TRUS guided biopsy and n = 110 patients (Group III) who underwent TRUS guided biopsy were compared. PIRADS scores of targeted lesions of mpMRI were correlated with the histopathological findings. Figure 1 (A-F) shows the result of 53-year-old patient with PSA level (39 ng/ml), mpMRI and MR guided Inbore prostate biopsy with Gleason score 8(4+4) PCa. The mean ADC showed significant difference between patients of PCa (0.56 ± 0.12 X 10−3mm2 /s), and patients with no evidence of cancer (1.0 ± 0.32 X 10−3mm2 /s) (Table 1). The PCa detection rate of mpMRI-Inbore biopsy was found 50 % (28/56) and for clinically significant cancer it was 93 % (26/28) while for mpMRI-TRUS guided biopsy 26 % (5/19). All the 5 patients of mpMRI-TRUS biopsy were found clinically significant cancer. The combined detection rate of techniques with and without mpMRI was also calculated and found 44 % (33/75), for mpMRI-Inbore biopsy and mpMRI-TRUS guided biopsy, for clinically significant cancer 93.9 % (31/33) while 34.5 % (38/110), in TRUS guided prostate biopsy and 73.6 % (28/38) for clinically significant cancer (Table 1). Clinically significant cancer having Gleason score 7 (3+4) or higher were included in study. Our study demonstrated that mpMRI accurately identified suspicious areas of lesion and helped to target these areas with accuracy for diagnosis of clinically significant cancer. The biopsy yields in mpMRI-Inbore biopsy 42.2% (140/331) and in mpMRI-TRUS guided biopsy 16.6% (46/276) while in TRUS guided prostate biopsy 27% (358/1320) were obtained as per the number of cores taken.
Discussion:
Our study demonstrated that, mpMRI-Inbore biopsy has higher detection rate of PCa, compared to mpMRI-TRUS guided biopsy and TRUS guided prostate biopsy2. The overall detection rate of combined mpMRI guided prostate biopsy was higher compared with TRUS guided prostate biopsy. The use of ADC may reduce the number of false positive findings as well as unnecessary biopsies cores. The detection rate using mpMRI was significantly higher in patients having PIRADS scores 4 and 5 than the patients of PIRADS score 3 and 2. Study shows that there is a significant advantage of mpMRI-Inbore biopsy compared to TRUS guided biopsy.
Conclusion:
mpMRI-guided Inbore biopsy showed better detection rate of PCa compared to two groups that is mpMRI-TRUS prostate biopsy and TRUS prostate biopsy.
Acknowledgements
NRJ thanks SERB, Government of India funding under FIST program (SR/FST/LSI-569/2013) and J.C. Bose Fellowship.References
1. Ahmed HU, et.al. PROMIS study group. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017 Feb 25;389(10071):815-822.
2. Wegelin O, et. al. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique? Eur Urol. 2017 Apr;71(4):517-531.
DOI: https://doi.org/10.58530/2023/0726