0722
Value of diffusion kurtosis MR imaging for evaluating response to first-line chemotherapy in unresectable pancreatic cancer1Shanghai Cancer Center, Shanghai, China, 2MR Application Development, Siemens Shenzhen Magnetic Resonance Ltd, Shenzhen, China, 3MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
Keywords: Pancreas, Diffusion/other diffusion imaging techniques
This study firstly compared diffusion kurtosis imaging (DKI) and traditional diffusion weighted imaging (DWI) in evaluating first-line chemotherapy in unresectable pancreatic cancer. The result demonstrated that higher efficacy was shown in DKI derived parameters than DWI by the ROC curve analysis. DKI has potential to become a new non-invasive tool for clinical efficacy evaluation and help clinicians select individualized treatment.Introduction
Pancreatic cancer is a malignant digestive tumor with poor prognosis. For those patients who are diagnosed at advanced stage losing their opportunity to undergo radical surgery, first-line chemotherapy regimens recommended by NCCN guidelines are used to prolong the survival period and improve the life of quality[1]. The purpose of our study was to compare the application of DKI and traditional diffusion weighted imaging (DWI) in evaluating chemotherapy efficacy in patients with unresectable pancreatic cancer.Methods
Patients fulfilling the following criteria were included in this study: 1) clinically diagnosed with unresectable pancreatic cancer; 2) without radiotherapy during the treatment phase; 3) underwent 3T MRI with both DKI and DWI sequence before and after chemotherapy; 4) the tumor size ≥ 2 cm; and 5) Eastern Cooperative Oncology Group performance status (ECOG PS) score of 0-1. Patients were excluded for incomplete standard treatment (severe adverse reaction, n=3; cytoreductive surgery n=1) or loss to follow-up (n=4). According to the recommendation of comprehensive guidelines for the diagnosis and treatment of pancreatic cancer, patients underwent the following first-line chemotherapy regimens: 1) gemcitabine combined with tegafur gimeracil oteracil potassium (GS): gemcitabine 1000 mg/m2 on Day 1 and Day 8, qd, intravenously; tegafur gimeracil oteracil potassium 60 to 100 mg, Day 1-15, bid, orally; every 3 weeks; and 2) gemcitabine combined with nab-paclitaxel (AG): nab-paclitaxel 125 mg/m2 and gemcitabine 1000 g/m2 on Day 1, Day 8, and Day 15, qd, intravenously, every 4 weeks.All MRI examinations were performed on a 3T scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) using a 16-channel phased-array volume coil as the receiving coil within 15 days before and after two courses of chemotherapy. The conventional DWI were obtained using a free-breathing single-shot echo-planar sequence (TR, 8,500 ms; TE, 56 ms; FOV, 381×309 mm2; matrix, 256×208; number of slices, 28; thickness, 5 mm; b values, 0, 50, 800 s/mm2, acquisition time, 2 min 40 s). The DKI sequence used the same scan parameters as the conventional DWI, except the b values (0, 100, 700, 1400, 2100 s/mm2). The acquisition time was 4 min 45 s.Measurement of DWI and DKI parameters Both conventional DWI parameters (ADC values) and DKI parameters (MD, MK) were obtained by using a post-processing research application (MR Body Diffusion Toolbox; Siemens Healthcare, Erlangen, Germany).ADC maps were calculated voxel-wise by fitting the DW images to a mono-exponential signal decay model[2, 3]:
S(b) = S0× exp (﹣b·ADC)
in which S(b) represents the signal intensity with diffusion weighting b, S0 represents the intensity without a diffusion gradient, and ADC represents the apparent diffusion intensity.The DKI parameters were generated voxel-wise by fitting the multi-b DWI to the diffusion kurtosis signal decay equation according to a two-variable linear least squares algorithm[4]:
S(b)=S0 × exp (﹣b·D +1/6·b2D2K)
in which D value represents the corrected diffusion coefficient , K value represents the diffusion kurtosis coefficient, indicating the degree to which the molecular motion deviates from the ideal Gaussian distribution model.
Statistical analysis The nonparametric Shapiro-Wilk test and the independent t test were adopted to compare the DWI and DKI parameters among different efficacy groups before and after the treatment. Continuous variables are expressed as the mean ± standard deviation. All statistical analyses were performed using SPSS software (version 22.0, Chicago, IL, USA) and MedCalc software (version 17.5.5, MedCalc Software, Ostend, Belgium). Dependent variables (PR=1, non-PR=0) (partial response, PR) and independent variables (DWI and DKI parameters) were selected for the construction of ROC curves. P<0.05 was considered statistically significant. ROC curve analysis was used to evaluated potential variables. Internal validity was assessed by use of bootstrapping procedure. ROC analyses were further performed to evaluate the diagnostic efficacy of each parameter in predicting the chemotherapeutic response of unresectable pancreatic cancer.
Results
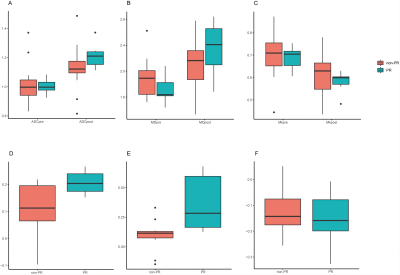
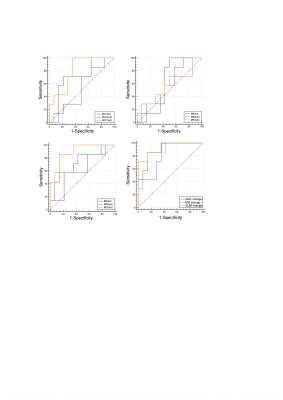
Statistics of functional parameters The ADCchange and MDchange in the PR group (0.21±0.05, 0.37±0.24) were significantly higher than those in the non-PR group (0.11±0.09, 0.10±0.12) (P=0.02, 0.002 repectively) (Figure 3). However, no statistically significant differences were shown between the PR group and non-PR group concerning certain aspects of ADCpre, ADCpost, MKpre, MKpost, MKchange, MDpre, and MDpost (P=0.734, 0.09, 0.686, 0.289, 0.573, 0.153, 0.166). The ICCs ranged from 0.857 to 0.912 for intraobserver agreement. The AUC of DWI and DKI parameters were successfully validated by 1000 times bootstrapping. The results of ROC curve analysis showed that MDchange (AUC=0.898) had greater diagnostic efficacy than ADCchange (AUC=0.80) (Figure 4). The MDchange had sensitivity of 85.7% and specificity of 85.7%, while the cutoff value was 0.1373. The combined model SUMchange (ADCchange+MDchange) showed higher AUC (0.912, P=0.002) than that of MDchange or ADCchange (Figure 4).Discussion and Conclusion
ADCchange and MDchange demonstrated strong potential for evaluating the response to chemotherapy in unresectable pancreatic cancer. MDchange showed higher specificity in the classification of PR and non-PR than ADCchange. Other parameters, including ADCpre, ADCpost, MKpre, MKpost, MKchange, MDpre, and MDpost, are not suitable for response evaluation. Further experiments are needed to evaluate the potential of DWI and DKI parameters in predicting the prognosis of patients with unresectable pancreatic cancer. DKI parameters have potential to be the new indicators for clinical efficacy evaluation while these results require further validation with a larger cohort.Acknowledgements
I would like to thank the following people who supported me with my present work.
To all the authors, Caixia Fu and Robert Grimm, for their teaching and massive help.
To my supervisor, Prof. Zhengrong Zhou, for his professional guidance.
References
[1]. Tempero, M.A., et al., Pancreatic Adenocarcinoma, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw, 2017. 15(8): p. 1028-1061.
[2]. Le Bihan, D., et al., MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology, 1986. 161(2): p. 401-7.
[3]. Le Bihan, D., et al., Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology, 1988. 168(2): p. 497-505.
[4]. Jensen, J.H. and J.A. Helpern, MRI quantification of non-Gaussian water diffusion by kurtosis analysis. NMR Biomed, 2010. 23(7): p. 698-710.
Figures
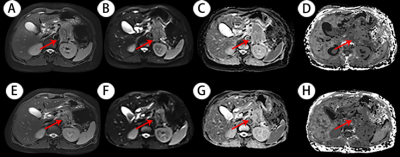
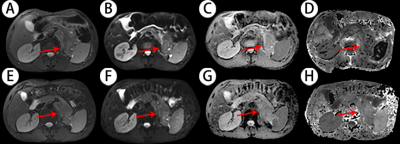
Figure 1. Representative example images of a 69-year-old patient with a 4.2×3.6 cm mass (red arrow) in the pancreatic tail before (A-D) and after (E-H) two courses of chemotherapy treatment. A and E: Axial half-Fourier-acquired single-shot turbo spin echo (HASTE) T2-weighted images; B and F: Diffusion weighted images (b=800); C and G: ADC maps; D and H: DKI maps. The ADC and MD values increased significantly, while the MK value decreased slightly after two courses of chemotherapy treatment. The lesion noticeably shrank after treatment, evaluated as PR according to the RECIST criteria.