0708
Prediction of Ischemic Stroke Based on Carotid Plaque VW-HRMRI Radiomics1Department of Magnetic Resonance, Lanzhou University Second Hospital, Lanzhou, China, 2Philips Healthcare, Xi’an, China
Synopsis
Keywords: Stroke, Radiomics, Carotid Plaque, Vessel Wall High-Resolution MRI
The study of the relationship between carotid atherosclerotic plaque and ischemic stroke must go beyond the assessment of the basic imaging characteristics of plaque or the degree of vascular stenosis, and should adopt a new model which carotid plaque imaging combined with artificial intelligence. This study established a radiomics model of carotid plaque based on vessel wall high-resolution MRI (VW-HRMRI) to accurately predict the risk of ischemic stroke. Our study showed that the radiomics_T1CE model and combined_T1CE model outperformed other models, whereas the combined model showed no significant difference with the radiomics model.
Introduction
Ischemic stroke is one of leading causes of disability and mortality worldwide, which seriously affects the long-term life quality of patients and brings heavy burden to patients and society. Carotid atherosclerosis has been recognized as the major cause of ischemic stroke[1]. At present, studies on the relationship between carotid atherosclerotic plaque and ischemic stroke mainly focus on the assessment of the basic imaging characteristics of plaque or the degree of vascular stenosis. Though computer aid diagnosis has been a major field of stroke related research, the inconsistent results make us difficult to develop an efficient prediction model[2]. Radiomics, aiming to extract mineable data from medical images, integrates digital imaging information, statistics, artificial intelligence, machine learning and deep learning methods to transform traditional visual imaging information into deep-level quantitative features for research[3]. This study established a radiomics model of carotid plaque based on vessel wall high-resolution MRI (VW-HRMRI) to accurately predict the risk of ischemic stroke.Methods
One hundred and twenty-seven patients with carotid plaque were enrolled in this study. They all received head MRI and VW-HRMRI that include 3D T1WI, and seventy-nine patients completed contrast-enhanced VW-HRMRI (3D-T1CE). Data were collected using a 3.0T MR scanner (Ingenia, Philips Healthcare, the Netherlands) with a 20-channel head-and-neck phase array coil. All the patients with carotid plaque were randomly divided into training and test cohorts. Basic imaging characteristics of the carotid plaques were measured and recorded, and combined with clinical metrics to build a traditional prediction model. Plaque segmentation for radiomics analysis was performed with an open-source software ITK-SNAP (version 3.8.0, www.itk-snap.org). Regions of interests (ROIs) were manually drawn layer by layer on 3D T1WI and 3D-T1CE images by two radiologists with 7 and 9 years of experience. Intraclass correlation coefficient (ICC) was used to find the inter-observer reproducibility. Radiomics features were then extracted on PyRadiomics platform. LASSO was applied to screen features, the final 10 versus 8 features were finally used to build radiomics_T1WI model and radiomics_T1CE model respectively. A combined model was established using traditional model and radiomics model. The AUCs value of ROC curves of all the models in prediction of ischemic stroke in the training and test cohorts were calculated respectively. To reduce overfitting, ten-fold cross validation was used in the training cohort to calculate the average AUC value. A nomogram of the combined model was established by the R software (version 3.5.0). All statistical analyses were performed using the R software and IBM SPSS Statistics software (version 25.0). P<0.05 was regarded as statistically significant.Results
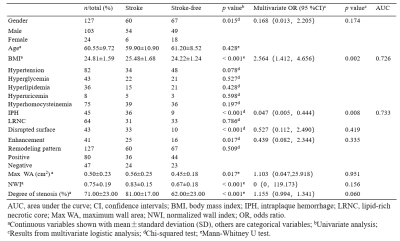
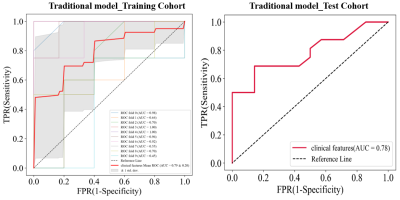
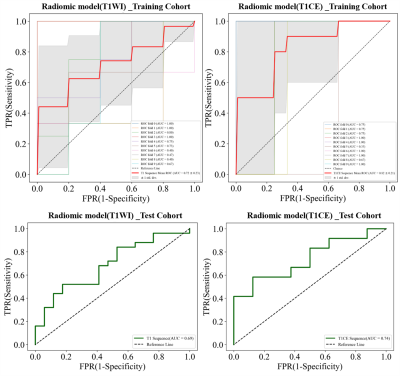
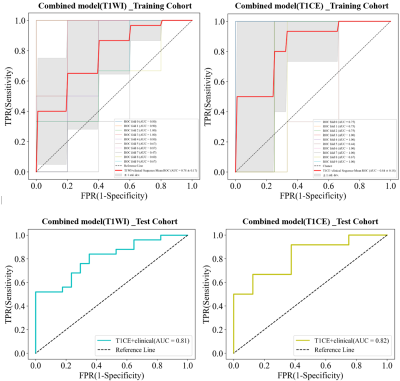
Traditional model: Of all the one hundred and twenty-seven enrolled patients, there were 60 stroke and 67 stroke-free patients. The demographic and clinical features were listed in Table1. Univariate analysis showed that gender, body mass index (BMI), intraplaque hemorrhage (IPH), disrupted surface, enhancement, maximum wall area (Max WA), normalized wall index (NWI) and degree of stenosis were significantly associated with stroke (p<0.05). Multivariate logistic regression analysis showed that BMI (OR=2.564; 95% CI,1.412–4.656) and IPH (OR=0.047; 95% CI,0.005–0.444) were independent predictors of ischemic stroke, and were used to build the traditional model, which achieved an AUC value of 0.79±0.20 versus 0.78 in the training and test cohorts (Fig.1). Radiomics model: In the training cohort, radiomics features on T1WI and T1CE images had AUC values of 0.72±0.23 and 0.82±0.21, while AUC values of the test cohort were 0.69 and 0.74 (Fig.2). Combined model: A combined model was finally constructed, and the nomogram was shown in Fig.3. Combined_T1WI model exhibited an AUC value of 0.78±0.17 versus 0.81 respectively in the training and test cohorts. Combined_T1CE model exhibited an AUC value of 0.84±0.18 versus 0.82 respectively in the two cohorts (Fig.4).Discussion
Radiomics can provide a large amount of quantitative data that cannot be evaluated visually by radiologist. In this study, we used the radiomics method to extract the plaque's radiomics features based on VW-HRMRI, and then combined with traditional features to accurately predict the risk of future ischemic stroke events. Our results showed that patients' BMI and IPH are associated with ischemic stroke, which is consistent with previous studies that certain carotid plaque characteristics, such as IPH and LRNC, are associated with increased risk of plaque rupture and distal cerebral embolism[4]. In addition, our study showed that the radiomics_T1CE model and combined_T1CE model outperformed other models, whereas the combined model showed no significant difference with the radiomics model. This comparison suggests that the traditional qualitative features might be covered, if not replaced, by quantitative descriptions by radiomics features. It further points out the potential of a more standardized diagnostic process based on objective quantitation[5].Conclusion
As an feasibility and exploratory study, this work showed that the radiomics_T1CE model of carotid plaque based on VW-HRMRI can accurately predict the risk of ischemic stroke. However, in the future, multicenter and large-scale data are needed to further determine the ability of this model predict ischemic stroke.Acknowledgements
Gansu Province Clinical Research Center for Functionaland Molecular Imaging (Project Number: 21JR7RA438).References
1. Mozaffarian, D., et al., Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation, 2015. 131(4): p. e29-e322.
2. Cao, X., et al., Normalized wall index, intraplaque hemorrhage and ulceration of carotid plaques correlate with the severity of ischemic stroke. Atherosclerosis, 2020. 315: p. 138-144.
3. Gillies, R.J., P.E. Kinahan, and H. Hricak, Radiomics: images are more than pictures, they are data. Radiology, 2016. 278(2): p. 563.
4. Saba, L., et al., Imaging biomarkers of vulnerable carotid plaques for stroke risk prediction and their potential clinical implications. The Lancet Neurology, 2019. 18(6): p. 559-572.
5. Zhang, R., et al., Identification of high-risk carotid plaque with MRI-based radiomics and machine learning. European Radiology, 2021. 31(5): p. 3116-3126.
Figures