0676
Widening access and increasing value to fetal MRI with a clinical 20min low-field 0.55T fetal exam in 40 participants1Center for the Developing Brain, School of Biomedical Engineering & Imaging Sciences, King's College London, London, United Kingdom, 2Biomedical Engineering Department, School of Biomedical Engineering & Imaging Sciences, King's College London, London, United Kingdom, 3Women's Health, Guy's and St. Thomas' NHS Foundation Trust, London, United Kingdom, 4Department for Diagnostic and Interventional Neuroradiology, Klinikum rechts der Isar Muenchen, Munich, Germany, 5Radiology, Guy's and St. Thomas' NHS Foundation Trust, London, United Kingdom, 6MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom
Synopsis
Keywords: Quantitative Imaging, Fetus
Comprehensive anatomical and functional fetal examination at low field (0.55T) MRI, obtained using a 20min protocol in 40 pregnant women demonstrates high quality data suitable for quantitative analysis both for anatomical radiological values and for functional T2* and diffusion values, all in-line with previously reported higher field values. It opens novel avenues and widens access to fetal MRI to new groups such as the fast growing fraction of obese and overweight pregnant women, in whom comprehensive assessment by screening ultrasound may be difficult.Introduction
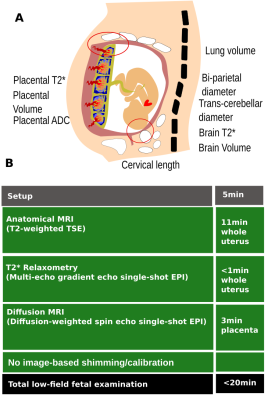
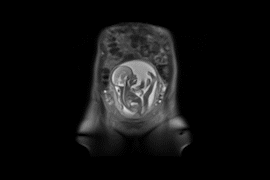
Fetal life is characterised by intricate and crucial development, deviations from which are associated with pathologies such as pre-eclampsia, fetal growth restriction (FGR), preterm birth and congenital anomalies, all of which carry risk of short and long-term maternal-fetal morbidity. In addition, the ongoing steep rise in obesity (with 29.5% of pregnant women in the US with a BMI>30 and 26.7% over 25, equating to 2.1 million pregnancies [1]) is associated with a further increase in complications and provides a challenging population rendering traditional Ultrasound and Doppler techniques less effective [1]. Early detection and comprehensive characterisation of abnormalities are however essential to antenatal and postnatal care.Widening the access to fetal MRI is thus important for these cohorts. A range of challenges of fetal MRI are closely linked to field strength such as susceptibility artefacts and resulting dynamic geometric distortion prominent around the tissue boundaries originating between fetal/placental tissue and the maternal bowel (see Figure 1A) and B1 inhomogeneities resulting in areas of reduced signal. Reducing field strength below the conventionally used 1.5T and 3T provides a beneficial operation point for these challenges, and offers in addition longer T2*, enabling longer read-out trains for the typically ssEPI based functional contrasts (T2* and Diffusion MRI [dMRI]), a larger dynamic T2* range relevant for reduced T2* in pathology and late gestation and reduced T1, decreasing slice-to-slice artefacts. Importantly, low-field allows larger bore size while maintaining good B0 homogeneity which increases maternal comfort and even more importantly widens access to fetal MRI to the above mentioned women with large BMI. In addition to previous fetal low field studies, the renaissance in low field imaging and the emergence of vendor-provided infrastructure allows exploitation of the latest technical developments in combination with the intrinsic properties of low field strength.
Methods
A 20min acquisition protocol was implemented on a clinical 0.55T scanner (MAGNETOM Free.Max, Siemens Healthcare, Erlangen, Germany) (see Figure 1B), consisting of the most widely used fetal contrasts [2-3] : T2-weighted 2D TSE stacks covering the fetus and uterus in six orientations (TR=2500ms, TE=106ms, FOV=450x450mm, 20 to 55 slices, resolution=1.5×1.5×4.5mm), diffusion-weighted single-shot dMRI (TR=7200ms, TE=129ms, FOV=400x400mm, 36 slices, resolution=3×3×3mm³, PF=6/8, b=[0,10,50,80,200,400,600,1000]s/mm2, 3 directions each), Multi-echo gradient echo (meGRE) to enable T2* relaxometry (TR=19170ms, TE=[46, 120, 194, 268, 342] ms, FOV=400x400mm, 50 slices, resolution=4x4x4mm, Grappa=2) of the placenta and fetal brain and finally a dynamic cine acquisition (TR=4000ms, TE=103ms, 30 dynamics, FOV=450x450mm, 1 slice, 2.8×2.8×10mm, Grappa=2, PF=5/8).Data was acquired after informed consent was obtained as part of an ethically approved study (MEERKAT, REC 19/LO/0852, Dulwich Ethics Committee) between May-October 2022 at St Thomas’ hospital, London. Women were scanned in supine position using the 6-channel blanket coil and 9-element posterior coil with continual heart rate and frequent blood-pressure monitoring and verbal interaction.
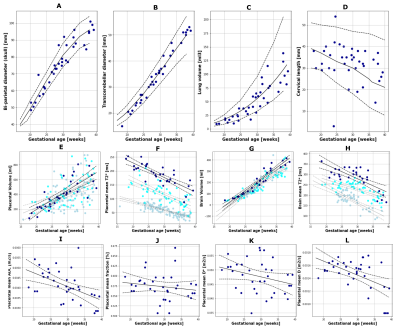
Conventional radiological measures including bi-parietal diameter, trans-cerebellar diameter, cervical length and lung volume were obtained from the TSE stacks by three experienced radiologists. The dMRI and meGRE data were fitted to standard mono-exponential decay functions. The dMRI data was also fitted to the IVIM model [4]. The placenta and brain were manually segmented to obtain mean quantitative values.
Results
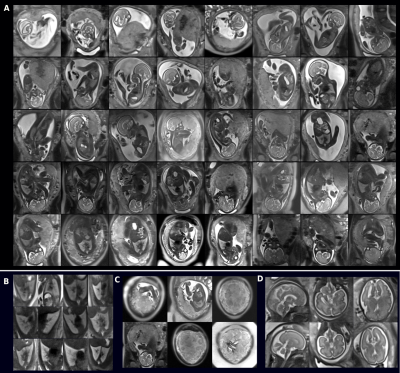
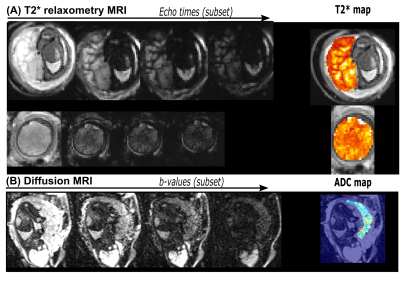
Anatomical data was obtained from all 40 participants (with only 2 stacks in one case due to claustrophobia) and functional data in 34 participants. See Figure 2 for a complete overview over the achieved anatomical data. The gestational age (GA) at scan ranged from 17-39 weeks (mean 28.92+-5.87) and the maternal BMI from 18.4, 40.53 kg/cm2 (mean 25.15+-4.72). Coronal whole-uterus TSE results from the whole cohort, zoomed for the fetal lungs and brains (Figure 1) and T2* and Apparent Diffusivity Coefficient (ADC) maps are shown and illustrate the high obtained quality (Figure 3). The radiological measures were well aligned with literature values [5-8], - literature trend lines added for reference in Figure 4A-D- and the functional measures displayed similar trends to high field data and significant correlation to GA (p<0.001 for placental T2* and brain T2* as well as placental ADC (4E-H), albeit higher absolute values for T2* as expected from lower field strength. Finally, high quality dynamic cine videos showing fetal limb motion, swallowing and cardiac activity (Figure 5) were obtained.Discussion and Conclusion
Contemporary low-field scanning provides several benefits for fetal MRI, importantly contributing to widening access to this diagnostic modality to the ever growing group of obese and overweight subjects, in whom comprehensive assessment by conventional US screening can be difficult. Next steps include expanding the study to further clinical groups. These may include a dedicated cohort of women with sub-diagnostic 20 week results and women with pre-eclampsia, FGR and gestational diabetes.Acknowledgements
The authors thank all pregnant women and their families for taking part in this study. The authors thank the research midwives and radiographers for their crucial involvement in the acquisition of these datasets. This work was supported by a Wellcome Trust Collaboration in Science grant [WT201526/Z/16/Z], a UKRI FL fellowship [MR/T018119/1] and by core funding from the Wellcome/EPSRC Centre for Medical Engineering [WT203148/Z/16/Z]. The views presented in this study represent these of the authors and not of Guy's and St Thomas' NHS Foundation Trust.References
[1] Creanga AA, Catalano PM, Bateman BT. Obesity in Pregnancy. N Engl J Med. 2022;387(3):248–259.
[2]A. Sørensen, J. Hutter, M. Seed, P. E. Grant, and P. Gowland, ‘T2*-weighted placental MRI: basic research tool or emerging clinical test for placental dysfunction?’, Ultrasound Obstet. Gynecol., vol. 55, no. 3, pp. 293–302, Aug. 2020, doi: 10.1002/uog.20855.
[3] P. J. Slator et al., ‘Combined diffusion-relaxometry MRI to identify dysfunction in the human placenta’, Magn. Reson. Med., vol. 82, no. 1, pp. 95–106, 2019, doi: 10.1002/mrm.2773
[4] Le Bihan, D. (1988), Intravoxel incoherent motion imaging using steady-state free precession. Magn. Reson. Med., 7: 346-351. https://doi.org/10.1002/mrm.1910070312
[5] Rypens F, Metens T, Rocourt N, et al. Fetal Lung Volume: Estimation at MR Imaging—Initial Results. Radiology. 2001;219(1):236–241.
[6] Masselli G, Perrone G, Kinkel K, et al. Are Second Trimester Apparent Diffusion Coefficient Values of the Short Uterine Cervix Associated with Impending Preterm Delivery? Radiology. 2016;280(3):897–904.
[7] Snijders RJ, Nicolaides KH. Fetal biometry at 14-40 weeks’ gestation. Ultrasound Obstet Gynecol. 1994;4(1):34–48.
[8] Chavez MR, Ananth CV, Smulian JC, Lashley S, Kontopoulos EV, Vintzileos AM. Fetal transcerebellar diameter nomogram in singleton gestations with special emphasis in the third trimester: a comparison with previously published nomograms. Am J Obstet Gynecol. 2003;189(4):1021–1025.
Figures