0642
Functional Connectivity of the Cerebellar Vermis in Bipolar Disorder
Vincent Magnotta1, Arshaq Saleem2, Gail Harmata1, Shivangi Jain2, Michelle W Voss3, Jess G Fiedorowicz4, Aislinn Williams3, Joseph J Shaffer5, Jenny Gringer Richards3, Ercole John Barsotti3, Leela Sathyaputri3, Samantha L Schmitz6, Gary E Christensen3, Jeffrey D Long3, Jia Xu3, and John A Wemmie3
1Radiology, University of Iowa, Iowa City, IA, United States, 2Psychological and Brain Sciences, University of Iowa, Iowa City, IA, United States, 3University of Iowa, Iowa City, IA, United States, 4University of Ottawa, Ottawa, ON, Canada, 5University of Kansas City, Kansas City, MO, United States, 6Des Moines University, Des Moines, IA, United States
1Radiology, University of Iowa, Iowa City, IA, United States, 2Psychological and Brain Sciences, University of Iowa, Iowa City, IA, United States, 3University of Iowa, Iowa City, IA, United States, 4University of Ottawa, Ottawa, ON, Canada, 5University of Kansas City, Kansas City, MO, United States, 6Des Moines University, Des Moines, IA, United States
Synopsis
Keywords: Psychiatric Disorders, fMRI (resting state)
This study used resting state functional connectivity to study connectivity of the cerebellar vermis with the cerebrum in bipolar disorder.
Introduction
Bipolar type I disorder is a major psychiatric disorder which significantly impacts the lives of approximately 1.0% of the population. The neural underpinnings of this disease are still unknown, but work to date has identified the emotional control network as being involved in the large mood swings that occur in this disorder. In addition, there is growing evidence that the cerebellum is also abnormal in the disorder. This has included observations of abnormal structure, function, and metabolism. Given these observations, we were interested in better understanding connectivity of the cerebellum with the cerebrum in bipolar disorder and if this connectivity changed with mood.Methods
This study enrolled 128 participants with bipolar type I disorder and 83 control comparison participants who completed an imaging session at 3T (Fig 1), which included anatomical imaging as well as ten minutes of resting state BOLD imaging. Data was analyzed using standard analysis pipelines and then a whole brain atlas was assembled by existing brain atlases for the cerebral cortex, subcortical structures, and cerebellum. Functional connectivity of the cerebellar vermis to all other brain regions was assessed to determine if there were differences between the participants with bipolar disorder and comparison control subjects. In addition, in the subjects with bipolar disorder we examined if there were relationships between functional connectivity and mood. We also explored if medication had an impact on the functional connectivity observed.Results
Functional connectivity of the cerebellar vermis in bipolar disorder was found to be significantly different (Fig 2) between the following regions as compared to controls: Vermis V to Left Pars Opercularis, Vermis V to Right Posterior Cingulate Gyrus (Schafer parcel X), Vermis V to Left Postcentral Gyrus, Vermis VIIIB to Left Postcentral Gyrus, Vermis VIIIB to Right Pre/Postcentral Gyrus, and Vermis X to Left Lateral Amygdala. All of the connections observed to be different between groups exhibited stronger connectivity in the participants with bipolar disorder with the exception of Vermis V to Left Pars Opercularis. In the participants with bipolar disorder, total scores from the MADRS scale was significantly associated with functional connectivity between the following regions (Fig 3): vermis IX to Left Ventroposterior Thalamus, vermis IX to Right Anterior Parahippocampal Gyrus, and Vermis X to Left Ventroposterior Thalamus. In the evaluation of YMRS scores to functional connectivity (Fig 3), a significant relationship between vermis X and left middle frontal gyrus was found. All of the associations with mood were negative meaning that increased mood ratings was associated lower functional connectivity between these regions. Associations with medication were found for the antidepressants and lithium with increased connectivity being associated with being on a particular class of medication.Conclusion
This study revealed significant differences in vermal connectivity in bipolar disorder to brain regions associated with emotion, language production, and motor function. The association between functional connectivity and mood in the participants with bipolar disorder all showed a decrease in connectivity associated with increased mood symptoms. The cerebellar vermis could be a key node in the emotional control network and future studies should consider expanding this network to include the cerebellum.Acknowledgements
This study was supported by funding from the National Institute of Mental Health (R01MH111578) with studies conducted on equipment (S10OD025025, S10RR028821) and facilities (UL1TR002537) supported by NIH. Some investigators received salary support from the Carver Foundation.
References
No reference found.Figures
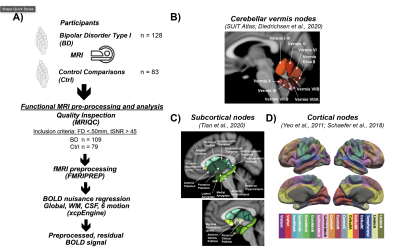
Fig 1. Study design. A) The study enrolled 128 participants with bipolar type I disorder and 83 frequency matched controls into a MR imaging study to assess differences in functional connectivity. After preprocessing, 109 participants with bipolar disorder and 79 controls were used in the statistical analysis. B) Functional connectivity of the cerebellar vermis (SUIT Atlas) with the cerebellum (SUIT Atlas), subcortical (Tian Atlas), and cortical (Shaefer Atlas) regions was assessed.
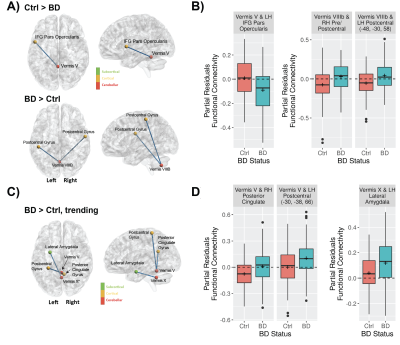
Fig 2. Differences in cerebellar vermal connectivity in bipolar type I disorder as compared to controls. A) Shows connections with significantly (FDR corrected q-value < 0.05) different connectivity in bipolar disorder. B) Shows the functional connectivity for the bipolar and control groups for the connections shown in A. C) Shows connections with trending (defined as uncorrected p-value < 0.001) differences connectivity differences in bipolar disorder as compared to controls. D) Shows the functional connectivity for the bipolar and control groups for the connections shown in C.
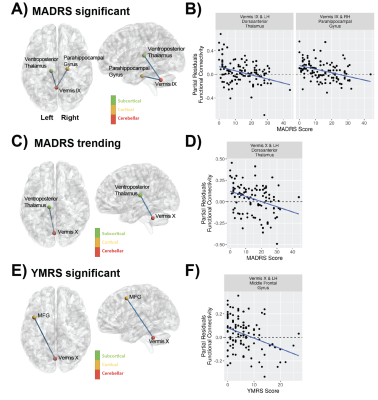
Fig 3. Mood as assessed with the MADRS and YMRS scales is associated with vermal connectivity in bipolar disorder. A) Vermal functional connectivity with a significant association with MADRS. B) Shows the regression between MADRS and functional connectivity. C) Vermal functional connectivity with (uncorrected p-value < 0.001) association with MADRS. D) Shows the regression between MADRS and functional connectivity. E) Vermal functional connectivity with a significant association with YMRS. F) Shows the regression between YMRS and functional connectivity.
DOI: https://doi.org/10.58530/2023/0642