0634
Deep-learning-based scoring for inflammatory lesions using SPARCC system1the university of HongKong, Hongkong, Hong Kong, 2Chiron Medical, HongKong, Hong Kong, 3the university of HongKong, HongKong, Hong Kong, 4Queen Mary Hospital, HongKong, Hong Kong
Synopsis
Keywords: Joints, Joints, deep learning, MRI, Ankylosing spondylitis
Our work proposed a work pipeline to automatic score the inflammatory lesion based on the SPARCC scoring system. This pipeline included the reference vessel intensity set-up, template-based registration, and lesion detection with scoring. With this pipeline, a time-saving and objective scoring method based on SPARCC scoring system could be achieved and widely applied to AS patient management. Our result showed reasonable performance for score-2 and score-3 lesions demonstrating the deep learning initial capacity of performing the SPARCC scoring.Introduction
MRI is an important diagnostic tool for ankylosing spondylitis (AS)1. The short tau inversion recovery (STIR)2 can visualize the inflammatory lesion on sacroiliac (SI) joints. The AS grade is correlated with the disease load, indicating the response to intraarticular steroid injection, and is associated with the histopathologic grade3. The Spondyloarthritis Research Consortium of Canada (SPARCC) provides a systematic scoring tool on the STIR images for the SI-joint3. However, manual scoring based on the SPARCC system is labor-intensive, time-consuming, reader-dependent, and requires special training. Deep learning, a subset of artificial intelligence (AI), could assist physicians in clinical scoring based on the SPARCC. SPARCC includes lesion size, zonal location, and relative intensity information. To our knowledge, this is the first deep learning study for automated SPARCC scoring on MRI.Method
Subject:228 MRI scans were involved for patients with diagnosed inflammatory lesions. In this study, we used 2D deep learning models; each slice was treated as an image. 1103 images and 225 inflammatory lesions were included in this study. The whole database was split into training and testing sets at the approximate ratio of 9:1. Individual patients only appear in training or testing sets.
Scoring Standard:
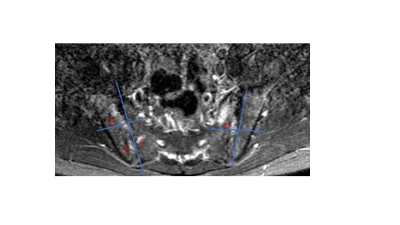
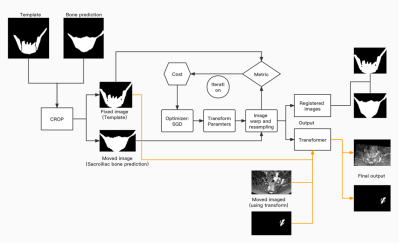
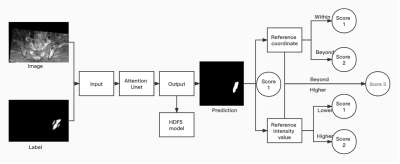
Based on the SPARCC system, the score 1 lesion appeared in only one quadrant area of a divided SI joint. The lesion that appeared in two quadrants or the lesion that appeared in one quadrant but the mean intensity was higher than the reference intensity value was defined as score 2. For score 3, the lesion appeared in two quadrants, and the mean intensity was higher than the reference intensity value.Figure 1 shows the example lesions with different scores. Frangi filter was used to detect the vessel structure4 automatically. Then, only the vessel with largest area in image was left for further calculating vessel reference intensity (fig 2).
MRI sequence:
A 3T MRI performed the STIR scans at oblique coronal orientations.
Data preprocess and Deep learning algorithms:
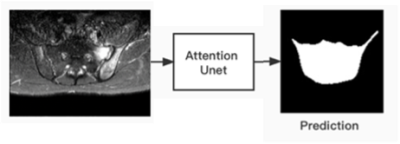
Attention Unet5, an algorithm derived from Unet6, was used. All deep neural networks were saved into HDF5 files.
Sacroiliac bone & Lesion segmentation:
A binary label (0 / 1) was used in segmentation. For the sacroiliac bone (fig 3), the ground truth region of interest (RoI) was the sacroiliac bone. Next, bounding boxes based on the result of the SI-bone segmentation were predicted. Later, images were cropped based on the generated bounding box. A template with 24 slices was used for separating the SI-joint into four quadrants, as shown in Figure 1. Every slice of the template was divided into four quadrants in each side. All scans were registered with the template slice-by-slice from the middle slice via a 2D linear registration. The original images and RoI images of the lesion were all registered with the template. Figure 4 shows the workflow of image registration. For the lesion segmentation (fig 5), the RoI was the lesion. Both original and RoI images were cropped based on the bounding box given by the prediction of SI-bone segmentation. If the predicted lesion crossed the dividing line of four quadrants, an extra one score was added. In addition, if the mean intensity of the predicted lesion was higher than the reference intensity value, an extra one score was added.
Statistical analysis:
The mode value was used to set the vessel intensity reference value. The mean value was used to calculate the mean intensity of the lesion. The Dice was used to measure the segmentation performance. The sensitivity and specificity were used to evaluate the scoring accuracy of each lesion.
Result
Only the image with lesions was used. Our lesions detection model had a sensitivity = 0.88 and specificity = 0.98, as reported previously7. The vessel intensity reference value was 0.63. The Dice of sacroiliac bone and lesion were 0.86 +/- 0.09 and 0.49 +/ - 0.28, respectively. The sensitivity and specificity for score 1 were 0.32 and 0.65; for score 2, they were 0.58 and 0.67; for score 3, they were 0.83 and 0.87, respectively.Dicussion
SPARCC scoring was the commonly used method for evaluating AS inflammation. It involves different measurements: lesion size, zonal location, and relative intensity. Manual SPARCC scoring had considerably large inter- or intra-reader variations8. In our work, we used deep learning model to detect the sacroiliac bone automatically and a template-based registration to determine the zonal location of the lesion. In addition, cropping to the sacroiliac bone region also reduced the background interference. While registering with a template could divide the sacroiliac bone based on the definition in the SPARCC system. The relatively high sensitivity and specificity indicated that the model could predict the lesion. Detecting the score-1 lesion was challenging due to the low intensity and small size. The relatively low Dice coefficient of lesion segmentation was mainly due to the mispredicted score-1 lesion. However, our model still showed reasonable performance for score-2 and score-3 lesions. Therefore, as the first study on the deep learning method for SI joint lesion scoring, the proposed pipeline showed the initial feasibility of the AI prediction of SPARCC score.Conclusion
The deep learning demonstrated the initial capacity of performing the SPARCC scoring.Acknowledgements
No acknowledgement found.References
1. Jürgen Braun, J.S., Ankylosing spondylitis. Lancet Digit Health, 2007. 369: p. 1379-90.2.
2. Rudwaleit, M., et al., Magnetic resonance imaging of the spine and the sacroiliac joints in ankylosing spondylitis and undifferentiated spondyloarthritis during treatment with etanercept. ANN RHEUM DIS, 2005. 64(9): p. 1305-1310.3.
3. Maksymowych, W.P., et al., Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis. ARTHRIT RHEUM-ARTHR, 2005. 53(5): p. 703-709.4.
4. Frangi A F, N.W.J., Vincken K L, et al., Multiscale vessel enhancement filtering[C]//International Conference on Medical Image Computing and Computer-Assisted Intervention. Springer Berlin Heidelberg, 1998: p. 130-137.5.
5. Ozan Oktay JS, L.L.F., Matthew Lee, Mattias Heinrich, Kazunari Misawa, Kensaku Mori, Steven McDonagh, Nils Y Hammerla, Bernhard Kainz, Ben Glocker, Daniel Rueckert., Attention U-Net: Learning Where to Look for the Pancreas. .
6. Olaf Ronneberger PF, T.B., U-Net: Convolutional Networks for Biomedical Image Segmentation. .
7. Lin, K.Y.Y., et al., Deep learning algorithms for magnetic resonance imaging of inflammatory sacroiliitis in axial spondyloarthritis.Rheumatology (Oxford), 2022.
8. Schwartzman, M.M.D. and WPMDF Maksymowych, Is There a Role for MRI to Establish Treatment Indications and Effectively Monitor Response in Patients with Axial Spondyloarthritis? Rheum Dis Clin North Am, 2019. 45(3): p. 341-358.
Figures