0626
Improved 3D DESS MR Neurography of the Lumbosacral Plexus with Deep Learning and Geometric Image Combination1Hospital for Special Surgery, New York, NY, United States, 2Chang Gung Memorial Hospital, Taipei, Taiwan, 3GE Healthcare, Waukesha, WI, United States
Synopsis
Keywords: Neurography, Neurography
Geometric image combination (GIC) and deep learning (DL) reconstructions were together applied to improve nerve visualization in lumbosacral plexus MR neurography (MRN) using the 3D dual echo steady-state free precession (DESS) sequence. Qualitative comparisons were made against standard image reconstruction of the 2nd echo of the DESS sequence. While standard-of-care (SOC) reconstructions of 3D DESS images provided effective vascular suppression and good nerve conspicuity, the DL-GIC reconstructed images demonstrated similar or improved nerve conspicuity.Introduction
Magnetic resonance neurography (MRN) typically uses 2D, T2-weighted sequences to provide high in-plane spatial-resolution (~0.6-0.8mm) for cross-sectional visualization of the lumbosacral plexus (LSP)1, at the expense of poor through-plane resolution (>3mm). To approach 3D isotropic spatial resolutions (~0.8-1.0mm) and appreciate curvilinear nerve trajectories, steady-state free precession sequences such as PSIF and DESS may be applied with water excitation (for fat suppression) and diffusion-sensitizing gradients (for vascular suppression)2,3. Although 3D DESS has been applied for peripheral nerve visualization in the head and neck region4, its potential for small LSP branch nerves has largely been unexplored due to insufficient SNR and long scan times to cover the whole pelvis. The DESS sequence simultaneously acquires two SSFP echoes, in which the 1st echo from free induction decay has higher signal but less T2-weighting, while the 2nd echo has lower signal but higher T2-weighting and vascular suppression. While these echoes may be combined using an average or sum of squares, they demonstrate suboptimal T2-weighting and vascular suppression. We propose application of a 3D deep learning (DL) reconstruction in 3D DESS MRN to reduce noise and improve image sharpness5. We also demonstrate an alternative method for combining both DESS echoes to enhance T2-weighting and SNR. We hypothesize that 3D DL with the proposed geometric image combination (DL-GIC) will improve nerve conspicuity in the LSP.Methods
The geometric-combined image Sgeo, is Sgeo=1/(1/S1+1/S2), where S1 and S2 are the image signals from the first and second DESS echoes, respectively. This simple equation preserves T2-weighting and vascular suppression of the lower-signal amplitude from S2, while utilizing both S1 and S2 for SNR. To compare SNR, nerve/fat and nerve/muscle contrast, signal simulations used standard DESS equations of nerve (T1/T2=1300/60ms), muscle (T1/T2=1400/35ms) and fat (T1/T2=400/160ms, fat saturation efficiency=90%), noise=5% and nominal TR/TE=15/5-10ms. Simulations were also used to determine the optimum flip angle (FA)6. A total of 17 patients (7F/10M, mean age=57, range=33-77 years) undergoing standard-of-care lumbosacral plexus MRN at 3T (Premier, GE Healthcare) provided written consent for this IRB-approved prospective study. A 3D DESS scan was acquired (Table 1). DL reconstruction (DLRecon)7 was performed separately on each echo on a separate workstation (Ubuntu 20.04 with Intel Xeon W-2265 CPU, Nvidia RTX A5000 GPU, ~2-minutes reconstruction time), followed by GIC processing using in-house software developed on Matlab. For qualitative evaluation, three board-certified radiologists graded two sets of DESS images on PACS (Sectra IDS7): 1) a ‘non-DL-GIC’ 2nd echo 3D image stack with standard-of-care (SOC) image reconstruction and 2) a ‘DL-GIC’ combined echo image stack. Images were graded on a 3–4-point scale separately by three readers for motion artifact (none, mild, moderate, severe), vascular suppression (none suppressed, large vessels only, small and large vessels) and conspicuity of proximal and distal segments of major, bilateral LSP branch nerves (sciatic, femoral, obturator, lateral femoral cutaneous) (no visualization, partial visualization with low confidence, partial visualization with high confidence, full visualization). Statistical analyses were performed using Wilcoxon signed-rank test. Inter-rater agreement was assessed using the ordinal-weighted, second order Gwet’s agreement coefficient (AC2). All statistical analyses were performed using R (version4.0.3). A p-value <0.05 was considered statistically significant.Results
Simulations showed that nerve SNR for GIC was higher than that of S2, and the nerve contrast for both GIC and S2 were higher than that from S1 and the average between S1 and S2. As nerve-to-muscle contrast increased but SNR decreased with flip angle (FA), the FA applied for in vivo scanning was 35o. Abnormal MR findings were identified in 12/17 subjects: non-specific nerve signal hyperintensity (7); intrinsic tumor (2); fracture-associated entrapment (1); radiation-induced neuropathy (1), neuropathy associated with auto-immune disease (1). DL-GIC provided equivalent vascular suppression and motion artifact compared to SOC images, and superior to equivalent nerve conspicuity for all branch nerves, with some raters grading the distal femoral and proximal obturator nerve segments as superior. Inter-rater agreement for nerve conspicuity was mostly similar between SOC and DL-GIC images (AC2: 0.41-0.89 and 0.44-0.90, respectively), but in four proximal nerve segments DL-GIC increased inter-rater agreement from moderate (0.41-0.60) to substantial (0.61-0.80).Discussion
While SOC DESS provided adequate vascular suppression and partial to full nerve conspicuity of most lumbosacral plexus nerves evaluated, images reconstructed with DL-GIC provided superior or equivalent nerve conspicuity, with equivalent or better inter-rater agreement. These preliminary results suggest DL-GIC DESS may provide consistently improved results for LSP MRN. While fat-suppressed fast-spin-echo techniques may also provide thin-section isotropic 3D LSP MRN8, DESS does not suffer from the blurring incurred by typically long FSE echo train lengths (>100) and may not require intravenous gadolinium for vascular suppression9. However, this work lacked of direct comparison between DESS and FSE. We also did not separately compare the effects of DL and GIC. Not all nerve segments could be visualized in all subjects due to variations in the acquired field-of-view, depending on the nerve(s) in question by the referring clinician. Furthermore, abnormal nerves were often more conspicuous; for example, with neuropathy, the lateral femoral cutaneous may be visualized in 90% of cases10, but visualization of the same nerve was inconsistent in our series likely because our cohort did not include patients with the imaging diagnosis of lateral femoral cutaneous neuropathy.Acknowledgements
HSS receives institutional research support from GE Healthcare.References
1. Chhabra, A., Rozen, S. & Scott, K. Three-Dimensional MR Neurography of the Lumbosacral Plexus. Semin Musculoskel R 19, 149–159 (2015).
2. Yoon, D., Biswal, S., Rutt, B., Lutz, A. & Hargreaves, B. Feasibility of 7T MRI for imaging fascicular structures of peripheral nerves. Muscle Nerve 57, 494–498 (2018).
3. Sveinsson, B. et al. Feasibility of simultaneous high‐resolution anatomical and quantitative magnetic resonance imaging of sciatic nerves in patients with Charcot–Marie–Tooth type 1A (CMT1A) at 7T. Muscle Nerve 66, 206–211 (2022).
4. Cruyssen, F. V. der et al. Magnetic resonance neurography of the head and neck: state of the art, anatomy, pathology and future perspectives. Br J Radiology 94, 20200798 (2021).
5. Zochowski, K. C. et al. Improvement of peripheral nerve visualization using a deep learning-based MR reconstruction algorithm. Magn Reson Imaging 85, 186–192 (2022).
6. Hardy, P. A., Recht, M. P., Piraino, D. & Thomasson, D. Optimization of a dual echo in the steady state (DESS) free‐precession sequence for imaging cartilage. J Magn Reson Imaging 6, 329–335 (1996).
7. Lebel, R. M. Performance characterization of a novel deep learning-based MR image reconstruction pipeline. Arxiv (2020).
8. Kasper, J. M. et al. SHINKEI—a novel 3D isotropic MR neurography technique: technical advantages over 3DIRTSE-based imaging. Eur Radiol 25, 1672–1677 (2015).
9. Zhang, Y. et al. Enhanced MR neurography of the lumbosacral plexus with robust vascular suppression and improved delineation of its small branches. Eur J Radiol 129, 109128 (2020).
10. Chhabra, A. et al. Meralgia paresthetica: 3-Tesla magnetic resonance neurography. Skeletal Radiol 42, 803–808 (2013).
Figures
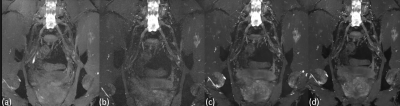
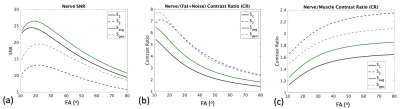
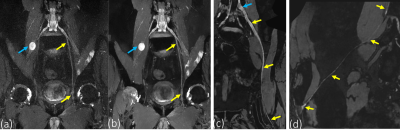
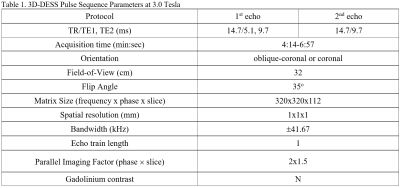
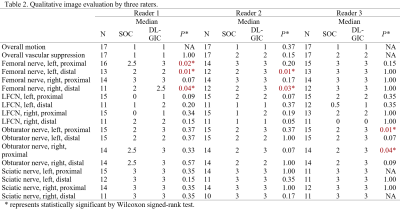
Table 2. Qualitative
image evaluation by three raters.
LFCN: Lateral femoral cutaneous nerve.
NA means the two groups are same (not included in statistical evaluation).
Motion artifact was graded as none (0), mild (1), moderate (2), severe (3).
Vascular suppression was graded as none (0), large vessels only (1), small and large vessels (2).
Nerve conspicuity was graded as no visualization (0), partial visualization with low confidence (1), partial visualization with high confidence (2), full visualization (3).