0625
Enhancing fluid signal in driven-equilibrium short-tau inversion-recovery (STIR) imaging with short TR times.
Constantin von Deuster1,2 and Daniel Nanz2,3
1Advanced Clinical Imaging Technology, Siemens Healthineers International AG, Zurich, Switzerland, 2Swiss Center for Musculoskeletal Imaging, Balgrist Campus AG, Zurich, Switzerland, 3University of Zurich, Zurich, Switzerland
1Advanced Clinical Imaging Technology, Siemens Healthineers International AG, Zurich, Switzerland, 2Swiss Center for Musculoskeletal Imaging, Balgrist Campus AG, Zurich, Switzerland, 3University of Zurich, Zurich, Switzerland
Synopsis
Keywords: MSK, Contrast Mechanisms, Driven Equilibrium
Fluid-sensitive Turbo-Spin-Echo (TSE) imaging in combination with Short-Tau Inversion Recovery for fat suppression (STIR) is commonly employed in musculoskeletal MRI. A Driven Equilibrium (DE) module following the imaging train can be used to reduce the Repetition Time (TR) without significant SNR loss. However, due to the STIR preparation, a conventional DE element rotates the fluid magnetization onto the negative z-axis instead of the positive z-axis, which delays longitudinal relaxation and attenuates the fluid signal. We implemented a modified DE module that increased fluid-signal intensity in STIR-TSE images of the spine.Introduction
T2 and PD weighted Turbo Spin Echoes (TSE) in combination with Short-Tau Inversion Recovery for fat suppression (STIR) are commonly employed in musculoskeletal MRI to delineate pathologies, e.g., myelopathy in the spinal cord1 or inflammation around metallic implants given the reduced sensitivity of the STIR technique to B0-inhomgeneity. This approach, however, suffers from long acquisition times due to the need for complete longitudinal magnetization recovery of fluid during one repetition time (TR). Multi-slice 2D acquisition with interleaved magnetization inversion and imaging part can mitigate this problem, however, such a straightforward solution is not possible in 3D STIR scans, where the slab- or non-selective radiofrequency (RF) pulses typically affect the whole imaged volume. In sequences without magnetization preparation, the recovery of longitudinal fluid magnetization can be accelerated by the application of a Driven Equilibrium (DE) or Fast Recovery (FR) module following the imaging train. Briefly, it uses a -90° pulse at the end of the echo train to flip remaining transverse magnetization onto the longitudinal axis which supports T1 recovery. This allows to shorten TR and reduce the acquisition time without significant loss of fluid SNR2.In contrast, a STIR preparation results in longitudinal fluid magnetization aligned along the negative z-axis at the time when the next excitation pulse is applied, since low-viscous fluids and most tissues have a longer T1 than fat (e.g. T1CSF / T1Fat = ~4200/360 ms @ 3 T3,4, CSF: cerebrospinal fluid). A conventional DE element delays longitudinal recovery and attenuates the fluid signal – instead of enhancing it - since it flips the remaining transverse magnetization onto the negative z-axis. In this study, we implemented a phase shifted flip-back pulse in the DE module and investigated its effect on fluid signal and image contrast in short-TR DE STIR images of the spine.
Materials and Methods
Figure 1 shows the STIR-TSE sequence with a state-of-the-art and a modified DE module. The modification consists of a phase change of the flip-back pulse by 180° relative to the state-of-art implementation: The modified flip-back pulse has a flip angle of 90° applied along the positive x-axis (+90°x) while the state-of-the-art implementation has a -90°x RF pulse2. The resulting pulse-sequence train can then be seen as a composite 0° pulse on longitudinal fluid magnetization, which drives its equilibrium. The proposed phase shift of the DE module was implemented in research application 2D and 3D STIR-TSE sequences and tested on a clinical 3-T MR-imaging system (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany, maximum gradient strength: 80 mT/m, maximum slew rate: 200 T/(msec)) using a 32-channel spine coil for posterior signal reception and an 18-channel surface coil for anterior coverage. Imaging was performed in sagittal orientation covering the lumbar spine of one healthy female subject (32 years, 60 kg). In the 2D case, additional images without DE were acquired as reference. The acquisition parameters are listed in Table 1. CSF and peri-spinal muscle signals (SCSF and SPSM, respectively) were measured in a manually placed circular ROI (50 mm2) at L3 level and signal ratios RFM = (SCSF / SPSM) reported as mean ± SD.Results
Figure 2 shows sagittal 2D STIR images of a lumbar spine acquired with an unusually short TR of 2340 ms at 3 Tesla. Note the low signal intensity of CSF when using a STIR without DE (Figure 2a), which is even reduced when using the state-of-the-art DE (Figure 2b). In contrast, using the proposed modification, higher CSF signal can be observed in the image (Figure 2c). RFM were low for the non- and state-of-the-art DE measurements (2.7±0.3 and 2.0±0.2, respectively) while the optimized DE technique provided the best CSF/muscle contrast: RFM = 3.9±0.4. Similar results were found in the 3D case as shown in Figure 3. With a TR of 1500 ms, RFM of the modified DE (RFM = 7.8±0.7) was increased by a factor of 2.8 compared to the state-of-the-art approach (RFM = 2.8±0.2).Conclusion
Our study showed that a modified DE module can successfully increase CSF signal and improve fluid/muscle contrast in STIR-TSE imaging. This enables acquisitions with significantly reduced TRs and hence shorter total acquisition times. Our approach requires only minor sequence modifications but has the potential to improve and accelerate T2 weighted STIR-TSE imaging of the musculoskeletal system.Acknowledgements
No acknowledgement found.References
1. Nouri A, Tetreault L, Singh A, et al. Degenerative cervical myelopathy: Epidemiology, genetics, and pathogenesis. Spine (Phila. Pa. 1976). 2015;40(12):E675–E693.
2. Bernstein M, King K, Zhou X. Handbook of MRI Pulse Sequences. 2nd ed. San Diego, United States: Elsevier Science Publishing; 2004.
3. Lin C, Bernstein M, Huston J, et al. Measurements of T1 relaxation times at 3.0T: implications for clinical MRA. Proc Intl Soc Mag Reson Med. 2001;9:1391.
4. Gold GE, Han E, Stainsby J, et al. Musculoskeletal MRI at 3.0 T: Relaxation times and image contrast. Am. J. Roentgenol. 2004;183(2):343–351.
Figures
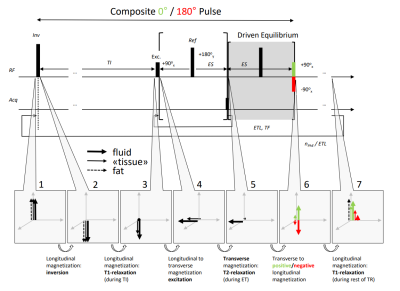
Figure 1: STIR-TSE sequence with modified (green) and conventional
(red) driven equilibrium (DE) module: The +90°/-90° flip-back pulse in
the modified/conventional DE module transforms the sequence to an
effective composite 0°/180° pulse on fluid magnetization, which drives/delays
its equilibrium and enhances/attenuates fluid signal. Inv: inversion pulse, TI: inversion time, Exc/Ref: excitation/refocusing pulse, ES: echo spacing, Acq: acquisition, ET: echo train, ETL:
echo-train length, TF: turbo factor, nPhE: number of phase-encoding
steps, TR: repetition time.
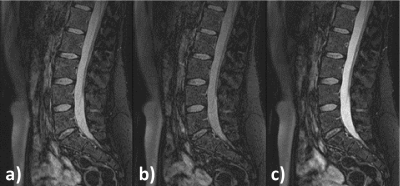
Figure 2: 2D STIR TSE images of a lumbar spine, acquired without a
driven-equilibrium flip-back pulse (a), with a conventional DE pulse-sequence
element, optimized for not magnetization-prepared sequences (b), and with the
modified DE element (c). Note the low signal intensity of the cerebral spinal
fluid (CSF) in a), which is even further reduced in b) in comparison with the increased
CSF brightness in c).
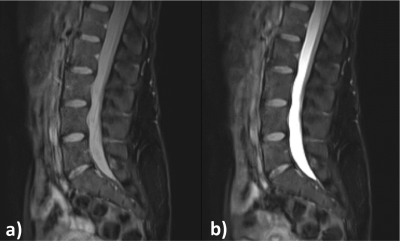
Figure 3: 3D STIR TSE images of a lumbar spine acquired with a TR time of 1500
ms, without a driven-equilibrium flip-back pulse (a) and with the modified,
phase-shifted flip-back pulse (b). Note the higher signal intensity of the
cerebral spinal fluid in b).
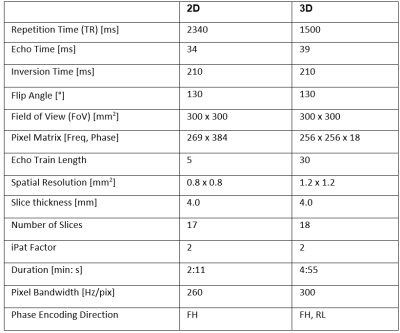
Table 1: MRI acquisition parameters for 2D and 3D TSE STIR sequences.
DOI: https://doi.org/10.58530/2023/0625