0600
Impacts of bone on the worst-case configuration for orthopedic implants under 1.5T and 3T MRI1Univ of Houston, Houston, TX, United States, 2HPC for MRI Safety, Jasper, GA, United States
Synopsis
Keywords: Safety, Bone
Due to the differences in both electrical and thermal properties, the RF-induced heating from implantable devices under MRI can have different behaviors inside muscle-like tissue and bone. A locally modified ASTM phantom with bone tissue was developed in the study. Simulations were used in the study to determine the worst-case heating configurations in the original and the modified ASTM phantoms. Based on our study, it was observed that the worst-case heating configuration can be altered when the devices are implanted in/near bone tissues. Consequently, additional in-vivo modeling would be required to understand the clinically relevant RF-induced heating.Introduction
Orthopedic implants are designed with dimensions and configurations to support patients with numerous anatomical structure variations. It is computationally expensive to evaluate RF-induced heating for numerous orthopedic implants inside heterogeneous human body phantoms under Magnetic Resonance Imaging (MRI). Instead, a simplified and homogeneous phantom is typically used to identify the worst-case heating configuration of orthopedic implants1. Previous studies have shown that the surrounding material/tissue can have a significant influence on the RF energy absorption of implants, especially for orthopedic implants2,3. The distinct difference in the electrical/thermal properties of bone and gelled saline has great potential to alter the worst-case configuration. Therefore, it is necessary to investigate the impact of modeling bone on the worst-case configuration of orthopedic implants.Methods
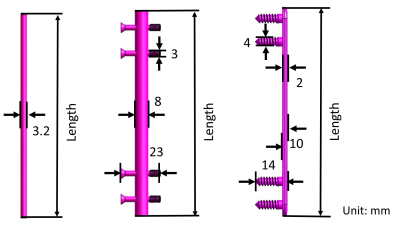
A customized phantom with a cylinder mimicking the bone inside the standard ASTM1 phantom is developed. The cylinder, with a diameter of 20 mm and a length of 460 mm, is 20 mm away from the phantom wall. Three implants, rod, nail, and plate are placed on, or inside, the bone according to the surgical protocol as shown in Fig. 1. The dimensions of implants are illustrated in Fig. 2 and their lengths are varied. The phantom is inside a generic G32 RF coil with the orthopedic implants located at the center. The G32 coil generates the same RF field as that inside a physical MR RF coil, i.e., a circularly polarized and uniformly distributed B1 field inside the coil. The operating frequency is 64 MHz at 1.5T and 128 MHz at 3T. For a tradeoff between the computational time and the resolutions, the mesh size of the phantom and bone is set to 2 mm, while the orthopedic implants have a smaller mesh size of 0.5 mm to ensure proper voxelization. Numerical simulations are performed by the Sim4Life software package.Results
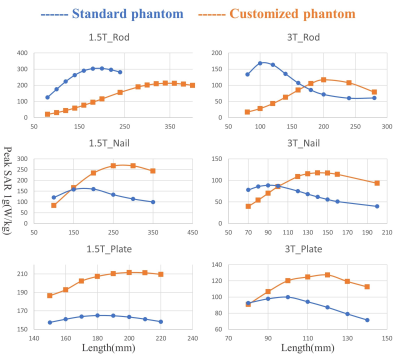
The RF-induced energy absorption, in terms of peak specific absorption rate spatially averaged over 1 gram (peak SAR1g), is evaluated for the orthopedic implants inside both standard phantom and customized phantom modeling the bone. The results are compared in Fig. 3. All the peak SAR1g are normalized to the limits of the normal operating mode with a whole-body averaged SAR of 2 W/kg. After placing a bone inside the standard phantom, the worst-case length of the rod increases from 190 mm to 350 mm at 1.5T and 110 mm to 200 mm at 3T. For the nail, the worst-case length varies from 175 mm to 275 mm at 1.5T and 90 mm to 140 mm at 3T. For the plate, the worst-case length changes from 180 mm to 200 mm at 1.5T and 100 mm to 120 mm at 3T.Discussion
When the rod is fully inserted inside the bone its surrounding materials are very different between the standard phantom and the customized phantom. The large difference in the electrical property of the bone and the gelled saline results in the 81% and 84% variations of the worst-case length at 1.5T and 3T, respectively. The nail is inside the bone, but the screws are exposed in the gel. Thus, the variations of worst-case length are less pronounced than that for the rod, which are 57% and 56% at 1.5T and 3T, respectively. For the plate the main part is inside the gel, while only its screws are inserted inside the bone. Consequently, there is only a slight difference in surrounding materials for plates inside the standard phantom and customized phantom which leads to 11% and 20% variations of worst-case length at 1.5T and 3T, respectively. Based on the discussions above, the variation of worst-case configuration for orthopedic implants highly depends on the relative position of the bone and the implants, i.e., how much of the implant is inside the bone.Conclusion
A customized phantom is developed by including a bone in the standard ASTM phantom. The RF-induced energy absorption for three orthopedic implants, the rod, the nail, and the plate, inside the customized phantom are compared with that inside the standard phantom. Our results confirm that the inclusion of bone in the worst-case assessment changes the worst-case configuration for orthopedic implants. Moreover, the variation depends on the relative position of the bone and the implants and the percentage of the implant volume inside the bone.Acknowledgements
The authors would like to thank Dr. Devashish Shrivastava at Columbia University for his comments and suggestions.References
1. ASTM F2182-19e2.(2019). Standard test method for measurement of radio frequency induced heating on or near passive implants during magnetic resonance imaging.
2. Xia, M., Guo, R., Zheng, J., & Chen, J. (2022, August). RF-induced Heating Evaluation for Passive Device in Tissue-Reduced Virtual Family Models at 1.5 T. In 2022 IEEE International Symposium on Electromagnetic Compatibility & Signal/Power Integrity (EMCSI) (pp. 610-613). IEEE.
3. Guo, R., Chen, M., Zheng, J., Yang, R., Chen, J., & Kainz, W. (2017, August). Comparison of in-vivo and in-vitro MRI RF heating for orthopedic implant at 3 Tesla. In 2017 IEEE International Symposium on Electromagnetic Compatibility & Signal/Power Integrity (EMCSI) (pp. 123-128). IEEE.