0594
Impact of Online Safety Screening on Outpatient MRI Workflow
Sheena Chu1,2, Elizabeth Briel2, John W Garrett2, Scott B Reeder1,2,3,4,5, and Ali Pirasteh1,2
1Department of Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Department of Radiology, University of Wisconsin-Madison, Madison, WI, United States, 3Department of Medicine, University of Wisconsin-Madison, Madison, WI, United States, 4Department of Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 5Department of Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
1Department of Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Department of Radiology, University of Wisconsin-Madison, Madison, WI, United States, 3Department of Medicine, University of Wisconsin-Madison, Madison, WI, United States, 4Department of Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 5Department of Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
Keywords: Safety, MR Value
MRI safety screening is required for all patients prior to their MRI exam. We aim to determine the impact of online MRI safety screening on delays and post-arrival cancellations. Time-to-image is the time between when the patient is paged in the waiting area and their first image acquisition. Post-arrival cancellations occur when the patient arrives but does not complete their MRI due to an unexpected safety or other issues (e.g., claustrophobia). We conclude that post-arrival cancellations and overall time-to-image decreased as a result of online MRI safety screening.
Keywords: Physics & Engineering: Safety, New Devices, MR Value
Introduction
All individuals must undergo safety screening prior to MRI. For those with pertinent history (e.g., an implanted medical device) additional information is required to determine whether MRI can be performed safely. Incomplete information can result in delays or cancellations after the patient has arrived at their appointment, leading to patient/staff dissatisfaction, delays in care, and lost revenue. Online safety screening prior to patient arrival has been demonstrated to reduce delays1. However, its efficacy in larger cohorts or in preventing post-arrival cancellations is unknown. The purpose of this work was to investigate the impact of online MRI safety screening on workflow delays and post-arrival cancellations in a large patient cohort using a data analytics platform.Methods
This was an IRB-approved retrospective study. Figure 1 summarizes our clinical MRI service workflow and the study setting. An online MRI safety screening questionnaire was made available via a patient web portal (MyChart, Epic) to all outpatients scheduled for an MRI. Independent of whether they complete the online screening, on the appointment day, all patients check in at the arrival desk and are given a pager. Once the technologist is ready to retrieve the patient from the waiting area, they notify the patient via the pager. The patient undergoes an in-person safety screening and any required pre-MRI preparatory procedures (e.g., IV placement) before entering the scanner room.Any delays in safety clearance (e.g., due to incomplete information about an implant) result in prolongation of the time between when the patient is paged and when the first set of images is acquired (time-to-image). Page time and first image time are automatically recorded (the former in the electronic health records and the latter in the image DICOM header), facilitating measurement of time-to-image for all patients. Furthermore, the number of patients who checked-in for their appointment but did not undergo MRI due to an unexpected issue (post-arrival cancellations) can also be identified through the EHR.
To assess the impact of online safety screening on time-to-image and post-arrival cancellations, data were retrospectively collected for all outpatient MRIs at a single facility for a 1-year period, starting at 3 months after online screening system implementation, to exclude the “ramp-up” period (Figure 2). Data were also collected for a 1-year period immediately prior to implementation of online screening. Average and standard deviation (SD) for time-to-image as well as the number of post-arrival cancellations were compared among three groups: (1) all patients before online screening (historical control), (2) patients who did not complete online screening after availability (synchronous control), and (3) those who completed online screening. Wilcoxon Rank, Kruskal–Wallis, F-test, and Z-tests were used to compare time-to-image and post-arrival cancellation rates, as well as differences of variance and proportion changes between groups. P<0.05 was considered significant.
Results
Table 1 summarizes the study results. From all 14,455 outpatient MRIs, 1,857 (13%) were excluded per following criteria: exams missing a timepoint, exams that were not the patient’s first MRI performed in a single appointment (only one screening is done per appointment), and exams that were not the patient’s first MRI in the data collection period. This yielded 5,641 exams before, and 6,957 exams after online screening implementation, of which 2,519/6,957 (36%) patients completed online screening. We saw no difference between average age and sex distribution of the different groups.Post-arrival cancellations were significantly lower in the online-screening group than the historical and synchronous control groups, respectively 0.52% vs. 1.33% vs 1.80%, P<0.001 (Table 1). Most common reasons for post-arrival cancellation are summarized in Figure 3, which demonstrates a decrease in cancellations among the online screening group due to metallic implants, patient pain/discomfort, and contrast allergy-related issues. Implant-related cancellations in the online screening group were not due to device-MRI safety, but due to a device check failure prior to MRI.
The online-screening group demonstrated a significantly lower average/SD of time-to-image than both the historical and synchronous controls (Table 1). There was a 1.9-minute decrease in average time-to-image and a 1.7-minute decrease in SD in the online screening group, compared to the historical control group. This resulted in a significant decrease in average/SD for time to image for the entire population after online screening implementation.
Discussion and Conclusion
We successfully investigated the impact of online MRI safety screening on workflow delays and post-arrival cancellations in a large patient cohort using a data analytics platform. Patients who completed an online questionnaire demonstrated a decrease in time-to-image and post-arrival cancellations compared to controls. Although the 1.9 min average time reduction may not seem significant, it is highly relevant from an operational standpoint, as the concurrent reduction in SD indicates a reduction in the number of outliers, which are the main reason for delays. While this may be due in part to selection bias, the observed difference in time-to-image across the entire patient population suggests otherwise. This study benefited from a large patient cohort, the use of analytics, and two control groups; limitations included its retrospective nature and inability to completely eliminate selection bias in the population that used online screening. In conclusion, online screening prior to MRI is a useful strategy to reduce workflow delays and post-arrival cancellations related to safety concerns.Acknowledgements
We wish to acknowledge support from GE Healthcare who provides research support to the University of Wisconsin and UW Health who provides research support for the UW MR2025 initiative. Dr. Reeder is the Fred Lee Sr. Endowed Chair of Radiology.References
- Pirasteh, A., VanDyke, M., Bolton-Ronacher, J., Xi, Y., Eastland, R., Young, D., Escobar, J., (...), Pedrosa, I. Implementation of an Online Screening and Check-In Process to Optimize Patient Workflow Before Outpatient MRI Studies (2016) Journal of the American College of Radiology, 13 (8), pp. 956-959.e5. http://www.elsevier.com/wps/find/journaldescription.cws_home/699814/description#description doi: 10.1016/j.jacr.2015.10.036
Figures
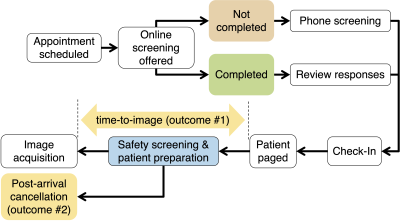
Figure 1: Summary of patient workflow and how the study outcomes (time-to-image and post-arrival cancellations) are defined.
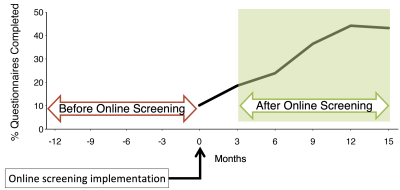
Figure 2: Utilization rate of online screening (% questionnaires completed) plotted against time, after online screening was implemented, demonstrates a ramp-up period, where utilization is relatively low for the first three months; this time period was excluded and data from the following 12-months were included for this study (green arrow). Data from 12 months prior to online screening implementation (red arrow) were used as a historical control.
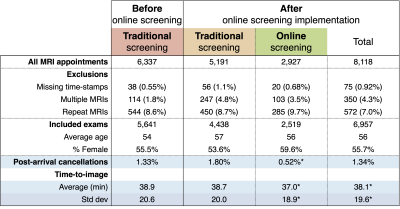
Table 1: Summary of patient demographics and study results. * = statistical significance.
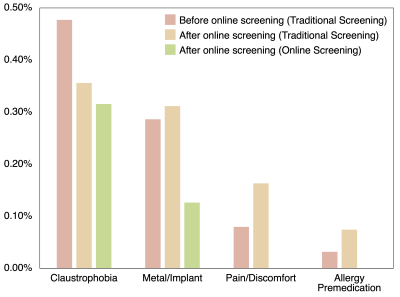
Figure 3: Most common causes for post arrival cancellations: Claustrophobia was the most common cause for cancellation, and even when reported on online screening, it was not adequately managed to avoid cancellation. There was a decrease in cancellations among the online screening group due to metal/implants, patient pain/discomfort, and contrast allergy-related issues. Implant-related cancellations in the online screening group were not due to device-MRI safety, but due to a device check failure prior to MRI.
DOI: https://doi.org/10.58530/2023/0594