0565
Predictive Value of Diffusion Magnetic Resonance Imaging for the Postoperative Outcome of Cervical Spondylotic Myelopathy1Department of Radiology, Peking University Third Hospital, BeiJing, China, 2Institute of Statistics and Big Data, Renmin University of China, BeiJing, China, 3MR Collaboration, Siemens Healthineers Ltd., BeiJing, China, 4Department of Orthopedics, Peking University Third Hospital, BeiJing, China
Synopsis
Keywords: Spinal Cord, Diffusion/other diffusion imaging techniques
This study used multi-factorial linear quantile mixed-effects regression models to predict the outcome of cervical spondylotic myelopathy (CSM) patients one year after surgery based on MRI. Six models were constructed using the linear quantile mixed model and linear mixed-effects regression model based on the diffusion magnetic resonance imaging (dMRI) data, all the imaging data (dMRI & Conventional MRI), and all the registered data (dMRI & Conventional MRI & clinical data). We found that fractional anisotropy (FA) values quantified by preoperative dMRI could predict the surgical outcome of CSM and showed a significant positive correlation with the postoperative outcome.
Introduction
Cervical spondylotic myelopathy (CSM) is one of the most common causes of adult spinal cord injury, and surgery is the primary treatment method. Preoperative prediction of which CSM patient will benefit from the surgery to identify suitable candidates is a topic of great clinical significance, as it can help clinicians better formulate treatment plans and improve patient prognosis.Few reports predicted the postoperative outcome of CSM based on diffusion MRI (dMRI). However, they are all based on single-factor analysis (1), ignoring the fact that the disease changes represented by different variables can jointly affect the outcome after surgery. In addition, the results of the published studies are controversial (2). Some studies reported that the fractional anisotropy (FA) value before surgery was significantly related to the modified Japanese Orthopaedic Association (mJOA) score three months after surgery (3), while other studies showed that FA and mean diffusivity (MD) values cannot predict postoperative efficacy (4). Nevertheless, it has been shown that diffusion tensor imaging (DTI) and neurite orientation disorder and identity imaging (NODDI) outperformed the traditional MRI methods, in terms of assessing postoperative function.
Therefore, this study aimed to use multi-factorial linear quantile mixed-effects regression models to explore the utility of dMRI in predicting the outcome of patients with CSM. Six models were constructed and compared using two multi-factorial linear quantile mixed-effects regression models based on three kinds of data, namely, dMRI data, all imaging data (dMRI & Conventional MRI), and all registered data (dMRI & Conventional MRI & clinical data).
Method
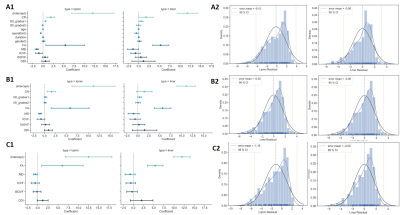
The data collection and simplified process pipeline of this study are shown in Figure 1.Data Acquisition
This study prospectively recruited 102 patients with CSM. The patients were followed up strictly according to the three-time points of 3, 6, and 12 months after the operation, and the mJOA score of the patients was obtained. Patients received scans on a 3T MRI scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) equipped with a 20-channel head/neck coil. Conventional MRI scans included the turbo spin echo (TSE) T1/T2WI and a T2 * weighted multi-echo gradient echo sequence (MEDIC). The dMRI images were obtained by zoomed imaging with the parallel transmission (ZOOMit) technique. The protocols for conventional MRI and dMRI are summarized in Table 1. Age, gender, surgical approach (anterior and posterior approaches), and duration of symptoms (months) were collected for all patients. The increased signal intensity (ISI) and compression ratio (CR) of the spiral core were manually measured based on the acquired conventional MR images.
Data Processing
The dMRI was processed with DTI and NODDI models using Python to obtain the FA, MD, isotropic volume fraction (ICVF), intellectual volume fraction (ISOVF), and orientation division index (ODI) parameters.
Statistics
The mJOA scores at three-time points (3, 6, 12 months) after the operation were compared by t-test and Kruskal-Wallis test. A total of nine continuous random variables, including preoperative mJOA, CR, age, symptom duration, FA, MD, ISOVF, ICVF, and ODI, were selected to calculate the correlation between the above variables and mJOA scores at three postoperative time points using distance correlation (dCorr), Pearson correlation (pCorr), and multiscale graph correlation (MGC), respectively. Correlations between four discrete random variables of preoperative mJOA grading, ISI grading, gender, and surgical modality and postoperative mJOA scores at three-time points were calculated using a t-test. The covariance between continuous random variables was calculated using pCorr. Correlation analysis was performed by the linear quantile mixed model (LQMM) and linear mixed-effects regression model (LMER), including all imaging variables (CR, ISI, and dMRI) and all continuous-type random variables, respectively. All statistical analyses were done in R and python. p<0.05 indicated a statistically significant difference.
Result
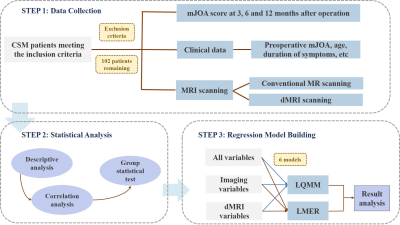
mJOA scores at different follow-up times (3,6, and 12 months) were statistically significant. The results of three single-factor correlation analyses of dCorr, pCorr, and MGC showed that the correlation between each variable and mJOA at different follow-up times was not high, and the nonlinear correlation was lower than the linear correlation, as seen in figure 2. There was no obvious collinearity between continuous random variables. Among the six models established by LQMM and LMER, the FA value had a significant positive correlation with mJOA scores at different times after operation, and the correlation was the strongest, as shown in figure 3.Discussion and Conclusion
In this study, a multi-factorial correlation analysis was performed in patients with CSM by linear quantile mixed-effects regression models, which showed that FA values were significantly and positively correlated with patients' mJOA scores at different postoperative follow-up times, indicating its utility to predict the beneficiaries of CSM surgery to identify good surgical candidates.Multi-factorial correlation analysis is more consistent with the actual disease situation and less influenced by subjectivity. Besides, DTI is a robust clinical diffusion imaging method. Thus, our findings suggested that the FA value quantified from dMRI data may be a good indicator to help preoperatively screen the candidates who can benefit from surgery and help with a timely change of treatment strategies for patients who may not see improvement.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (82102638 and 82171927).
References
1. Kara B, Celik A, Karadereler S, et al. The role of DTI in early detection of cervical spondylotic myelopathy: a preliminary study with 3-T MRI [J]. Neuroradiology, 2011, 53(8): 609-16.
2. Shabani S, Kaushal M, Budde M D, et al. Diffusion tensor imaging in cervical spondylotic myelopathy: a review [J]. Journal of neurosurgery Spine, 2020, 1-8.
3.Vedantam A, Rao A, Kurpad S N, et al. Diffusion Tensor Imaging Correlates with Short-Term Myelopathy Outcome in Patients with Cervical Spondylotic Myelopathy [J]. World neurosurgery, 2017, 97(489-94.
4.Rajasekaran S, Kanna R M, Chittode V S, et al. Efficacy of Diffusion Tensor Imaging Indices in Assessing Postoperative Neural Recovery in Cervical Spondylotic Myelopathy [J]. Spine, 2017, 42(1): 8-13.
Figures
Study flow chart. The process of this study is divided into three parts: data collection, data analysis, and regression model building.
CSM, cervical spondylotic myelopathy; dMRI, diffusion MRI; LMER, linear mixed-effects regression model; LQMM, linear quantile mixed model; mJOA, modified Japanese Orthopaedic Association.

(A) dCor, pCor, and MGC results of the continuous random variables. (B) The t-test results of discrete random variables. The correlation between any variable and mJOA at different follow-up times was not high in the single-factor analysis. The linear correlation was stronger than the nonlinear correlation.
CR, compression ratio; dCorr, distance correlation; pCorr, Pearson correlation; MGC, multiscale graph correlation; FA, fractional anisotropy; ICVF, isotropic volume fraction; ISOVF, intellectual volume fraction; MD, mean diffusivity; ODI, orientation division index.