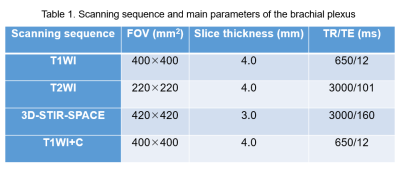
0476
The value of Cinematic Volume Rendering Technique: magnetic resonance imaging in diagnosing tumors around the brachial plexus1Department of Magnetic Resonance, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 2MR Collaborations, Siemens Healthineers Ltd., Beijing, China
Synopsis
Keywords: Visualization, Nerves, Cinematic Volume Rendering Technique (cVRT);Brachial plexus nerve
Cinematic Volume Rendering Technique (cVRT) can clearly display the contours of the tumor, brachial plexus, and peripheral blood vessels, and the extent of their involvement while simultaneously imaging them. The three-dimensional anatomical effect is more realistic, playing a direct role in guiding the surgical plan.Introduction
The brachial plexus is a complex anatomical structure that may be invaded by surrounding tumors, affecting its function1. Magnetic resonance imaging is the best non-invasive way to diagnose brachial plexus tumors2-5. The 3D-STIR-SPACE sequence can show the location, origin, and scope of brachial plexus-related peripheral tumors. It can be reconstructed in three dimensions through post-processing to clearly show the spatial positional relationship between the tumor and the brachial plexus. However, the 3D-STIR-SPACE sequence has certain limitations in demonstrating the wrapping and infiltration of brachial plexus-related tumors6-9. This study aimed to explore the diagnostic advantages and clinical application value of the Cinematic Volume Rendering Technique (cVRT) to evaluate the relationship between the brachial plexus and peripheral tumor lesions and blood vessels.Methods
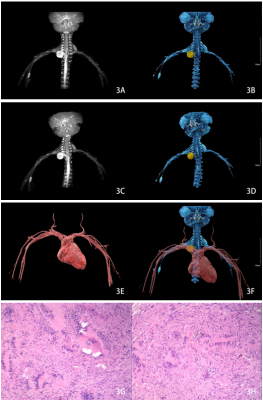
This study included 71 patients with brachial plexus tumors. All patients were examined on Siemens 3.0T MRI scanner, and T1WI, T2WI, 3D-STIR-SPACE, and T1WI enhanced sequences were collected. All images were analyzed by two attending physicians specializing in neuroimaging diagnosis. When there were differences of opinion, an agreement was reached after consultation. The tumor site, size, morphology, signal characteristics of all patients, and their relationship with the brachial plexus and surrounding structure were summarized. The 3D-STIR-SPACE sequence was used to image the brachial plexus nerves, and the sequence image data were transmitted to the syngo.via VB40(Siemens Healthcare, Erlangen, Germany)for processing. After MIP reconstruction of the brachial plexus nerves, soft tissues such as muscles were reduced to decrease interference with the anatomical positional relationship between the tumor and the brachial plexus nerves. After the tumor MPR was reconstructed, the tumor range was sketched layer by layer, the brachial plexus nerve fused with the tumor image, and cVRT was used to render and obtain a three-dimensional model, which clearly showed the location and tissue structure of the brachial plexus nerves and the tumor in all directions. The three-dimensional image of blood vessels was obtained in the same way. Finally, the three-dimensional images of the brachial plexus and tumor were fused with the three-dimensional images of the blood vessels. To better observe the relationship between the three, the transparency of the blood vessel image was adjusted to 65%.Results
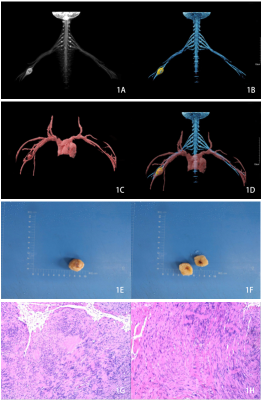
From November 2012 to July 2022, 71 patients (mean age 47.1 years, 33 males, 38 females) with tumors around the brachial plexus were enrolled. The brachial plexus, tumors, and blood vessels of all patients were well-displayed by cVRT. Among them, 37 patients had tumors that grew along the brachial plexus on one or both sides that were spindle-shaped, spherical, or had multiple beads. The tumors of seven patients pushed against the brachial plexus and were round, lobulated, or irregular, whereas sixteen had a spherical tumor surrounding the brachial plexus. In addition, the tumors in eleven patients showed irregular infiltration of the brachial plexus. The maximum diameter of all tumors ranged from 1 to 10 cm (average, 4.4 cm). The tumor showed moderate homogeneous or heterogeneous signal on T1WI, a high or low mixed signal on T2WI, and homogeneous or heterogeneous enhancement.Discussion
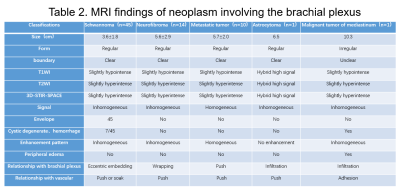
Tumors associated with the brachial plexus nerve area are usually completely removed by surgery. A comprehensive assessment is required before operating or the brachial plexus nerves become easily damaged during the procedure10, 11. Therefore, this study tried to use cVRT based on 3D-SPACE-STIR brachial plexus imaging, combined with enhanced MRI, to obtain a three-dimensional fusion image of the tumor, brachial plexus nerves, and blood vessels after processing. Different color levels are used to distinguish the three tissues. In this model, the spatial and positional relationship between the tumor, brachial plexus nerves, and blood vessels can be well reflected.Of the 71 patients in this study, 46 were treated surgically and 25 conservatively. In Case 1, a 42-year-old female, the three-dimensional fusion image obtained after treatment with cVRT technology showed that the brachial plexus nerve traveled through the tumor. The tumor was closely related to the brachial plexus nerve. The trunk of the right brachial artery was displaced downward under pressure. In addition, the branches of the brachial artery had small arteries that supplied blood to the tumor. The operation was difficult. Gentle manipulation was used during the surgery to separate the branches of the brachial artery around the tumor to avoid damage to the brachial plexus nerve. The tumor was slowly cut with minor bleeding, consistent with the results of the imaging examination, and the tumor was completely removed. The patient recovered well after the operation. In three dimensions, magnetic resonance was used to develop and reconstruct the tumor, brachial plexus nerves, and blood vessels. We obtained a three-dimensional model of the tumor involving the brachial plexus nerves and blood vessels and formulated the surgical approach and method. The process went smoothly, the surgical time was shortened, and the patient's symptoms improved significantly after the operation.
Conclusion
CVRT can clearly show the origin of tumors around the brachial plexus and the relationship with the nerves and peripheral blood vessels, providing reliable information for clinical diagnosis and treatment.Acknowledgements
We wish to thank Dr. Yanglei Wu in MR Collaborations, Siemens Healthineers Ltd. for technical guidance.References
1. Tharin B D, Kini J A, York G E, et al. Brachial plexopathy: a review of traumatic and nontraumatic causes[J]. AJR Am J Roentgenol, 2014,202(1):W67-W75.
2. Somashekar D, Yang L J, Ibrahim M, et al. High-resolution MRI evaluation of neonatal brachial plexus palsy: A promising alternative to traditional CT myelography[J]. AJNR Am J Neuroradiol, 2014,35(6):1209-1213.
3. Upadhyaya V, Upadhyaya D N, Kumar A, et al. Magnetic resonance neurography of the brachial plexus[J]. Indian J Plast Surg, 2015,48(2):129-137.
4. Amrami K K, Felmlee J P, Spinner R J. MRI of peripheral nerves[J]. Neurosurg Clin N Am, 2008,19(4):559-572.
5. Wade R G, Takwoingi Y, Wormald J, et al. MRI for Detecting Root Avulsions in Traumatic Adult Brachial Plexus Injuries: A Systematic Review and Meta-Analysis of Diagnostic Accuracy[J]. Radiology, 2019,293(1):125-133.
6. Vargas M I, Viallon M, Nguyen D, et al. New approaches in imaging of the brachial plexus[J]. Eur J Radiol, 2010,74(2):403-410.
7. Viallon M, Vargas M I, Jlassi H, et al. High-resolution and functional magnetic resonance imaging of the brachial plexus using an isotropic 3D T2 STIR (Short Term Inversion Recovery) SPACE sequence and diffusion tensor imaging[J]. Eur Radiol, 2008,18(5):1018-1023.
8. Tagliafico A, Succio G, Neumaier C E, et al. Brachial plexus assessment with three-dimensional isotropic resolution fast spin echo MRI: comparison with conventional MRI at 3.0 T[J]. Br J Radiol, 2012,85(1014):e110-e116.
9. Zhang L, Xiao T, Yu Q, et al. Clinical Value and Diagnostic Accuracy of 3.0T Multi-Parameter Magnetic Resonance Imaging in Traumatic Brachial Plexus Injury[J]. Med Sci Monit, 2018,24:7199-7205.
10. Penkert G, Carvalho G A, Nikkhah G, et al. Diagnosis and surgery of brachial plexus injuries[J]. J Reconstr Microsurg, 1999,15(1):3-8.
11. Martin E, Senders J T, DiRisio A C, et al. Timing of surgery in traumatic brachial plexus injury: a systematic review[J]. J Neurosurg, 2018:1-13.
Figures